Can brain cooling revolutionise stroke treatment?
A stroke is a life-threatening condition in which oxygen is prevented from reaching the brain, causing brain cells to die. At Western University in Canada, Dr Ting-Yim Lee, a biomedical engineer, has teamed up with Dr Marat Slessarev, a clinical doctor, to develop an innovative new device that can cool a stroke patient’s brain, thereby reducing the amount of damage caused.
Talk like a biomedical engineer
Cerebral blood flow — the measure of how much blood flows through the brain to deliver oxygen to brain cells
Metabolic coupling — when brain activity increases, cerebral blood flow increases to supply the extra oxygen needed by active brain cells
Metabolic processes — the chemical reactions in cells which create the energy necessary for life
Microprocessor-based controller — a controller that uses a tiny computer chip to control and monitor its actions
Randomised controlled trial — a clinical study to test a new medical intervention, in which patients are randomly assigned to either receive the intervention or a standard ‘control’ treatment
Stroke — a medical condition caused when blood supply to part of the brain is interrupted or reduced, depriving brain tissue of oxygen
Every two seconds, somewhere in the world, someone suffers a stroke. According to the World Health Organization (WHO), stroke is the second leading cause of death worldwide, claiming millions of lives each year and leaving countless others with disabilities. Dr Ting-Yim Lee, a medical imaging scientist, and Dr Marat Slessarev, a clinical doctor, both based at Western University, are investigating whether brain cooling could be a ground-breaking approach to stroke treatment. Together, they have designed and are now testing a new medical device which can cool a patient’s brain by delivering cold air through their nostrils.
What is cerebral blood flow?
Cerebral blood flow is the measure of how much blood the brain receives. This circulation is vital for brain function as it delivers oxygen to sustain its metabolic processes. “If the brain is deprived of blood flow, such as during a stroke, then brain cells will start to die, and irreversible brain injury may occur,” explains Marat. “If this injury is too large, the patient’s brain function may be limited, or the injury may even progress to brain death.”
Cerebral blood flow regulates the brain’s temperature through two main mechanisms. Firstly, if brain activity increases it will generate heat. This leads to an increase in blood flow to supply additional oxygen. “This process is known as metabolic coupling, which not only supports brain function but also helps to manage the heat produced,” explains Ting. Secondly, the blood circulating into the brain can transfer heat to or from the rest of the body. For instance, when the blood entering the brain is cooler than the brain itself, it lowers the brain’s temperature.
How can brain cooling help stroke patients?
“Lowering the brain’s temperature can reduce its need for oxygen by slowing down the brain’s metabolic processes,” explains Ting. As cerebral blood flow is reduced during a stroke, lowering brain temperature can lessen the injury caused by the lack of oxygen in the brain. Cooling the brain can also reduce inflammation, remove harmful molecules that build up when the brain does not get enough oxygen, and stop excess water from leaking into the brain from blood vessels, which can prevent it from swelling.
How do Ting and Marat cool brains?
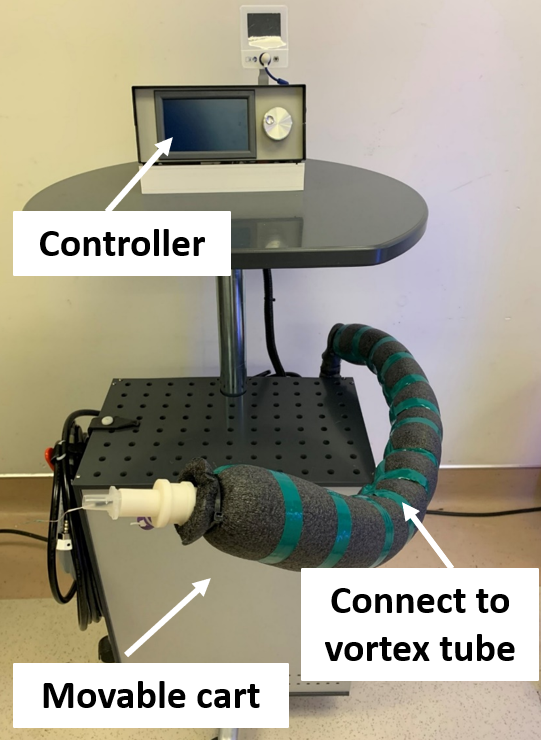
Ting, Marat and their team have developed the Vortex tube IntraNasal Cooling Instrument (VINCI), a new medical device designed to cool the brain and improve stroke recovery outcomes. It consists of a metallic tube with grooves along its length to generate cold air that is then piped into the nostrils via soft flexible tubing. “When compressed air is introduced through an inlet on the side of the tube, these grooves split the air into two streams: one hot and one cold,” explains Ting. “At the cold end, a valve regulates the flow and temperature of the cold air. Notably, decreasing the flow rate of the cold air also lowers its temperature.”
How did the team design and test VINCI?
Reference
https://doi.org/10.33424/FUTURUM506
The development of VINCI presented several challenges for the team. “Our first challenge was to develop a microprocessor-based controller that could automatically adjust the flow rate and temperature of cold air based on the brain’s temperature,” explains Ting. This controller had to operate effectively across three critical phases of the cooling treatment. Initially, the brain’s temperature is rapidly cooled to 2-4 °C below normal, before being maintained at this temperature for 18 to 24 hours. After treatment, the brain must be rewarmed very slowly to prevent any shock or additional stress to the brain. “We also need to ensure that the body’s temperature doesn’t fall below the point where shivering begins,” says Ting. “This is important because when we cool the brain, the blood that circulates from the brain back to the rest of the body is colder, which can lower the overall body temperature.”
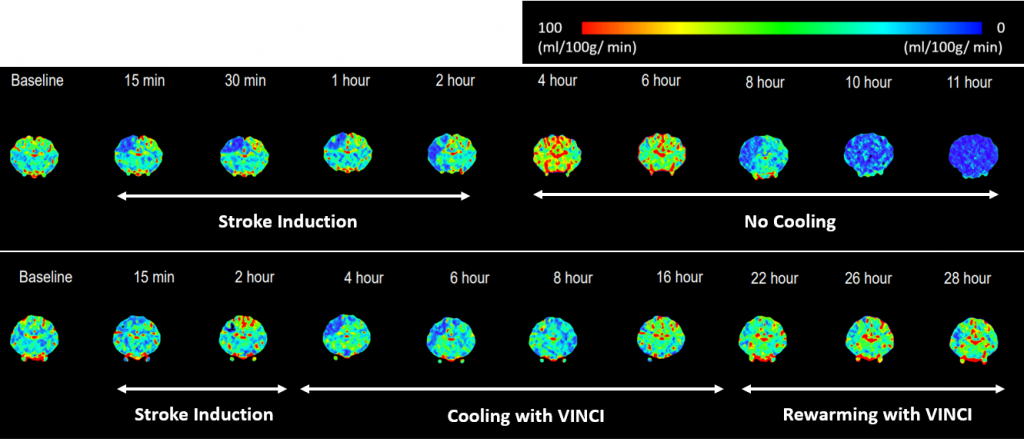
To investigate the effectiveness of brain cooling for reducing post-stroke brain damage, the team tested VINCI on pigs. Strokes were induced in two groups of pigs, one of which then received brain cooling treatment while the other did not. The results of this experiment showed a remarkable improvement in survival rates in pigs that had their brain cooled: only 23% of untreated pigs survived the stroke, while 75% of treated pigs survived. These findings highlight the promising potential of brain cooling with VINCI as a therapeutic intervention to enhance survival rates and mitigate adverse effects following a stroke.
What next for VINCI?
Having conducted successful tests on pigs, the next step is to test VINCI on human volunteers to ensure it works as intended during the three key phases of cooling treatment. These clinical trials will also reveal any potential side effects when using VINCI on humans, ensuring its safety and efficacy for clinical use. “From a clinical perspective, we have to demonstrate that it is feasible to use VINCI in clinical settings,” explains Marat. “We will then follow up with randomised controlled trials to assess if brain cooling improves patient outcomes, like brain function and survival rate.” It is these rigorous investigations that will pave the way towards establishing VINCI as a routine clinical treatment for stroke patients, offering hope for improved outcomes and enhanced recovery.
 Dr Ting-Yim Lee
Dr Ting-Yim Lee
St. Joseph’s Health Care London, Lawson Research Institute, Canada
Robarts Research Institute and Medical Biophysics, Western University, Canada
Fields of research: Medical imaging, biomedical engineering
Dr Marat Slessarev
London Health Science Centre, Lawson Health Research Institute, Canada
Department of Medicine, Western University, Canada
Field of research: Critical care medicine
Research project: Developing a brain cooling device to improve the outcomes for stroke patients
Funder: Canadian Institutes of Health Research (CIHR)
About biomedical engineering
Biomedical engineering stands at the intersection of engineering, biology and medicine, aiming to revolutionise healthcare by developing innovative solutions to complex medical challenges. Medical imaging plays a key role, as imaging techniques are used to monitor the performance of designed devices. This interdisciplinary field combines principles from physics, mathematics and engineering sciences and applies them to the study of biological systems, with the ultimate goal of improving patient care, advancing medical technology and enhancing our understanding of human health.
Collaborative expertise driving innovation
Within the fields of biomedical engineering and medical imaging, collaborations between researchers from diverse backgrounds often lead to ground-breaking discoveries. Ting, a medical imaging scientist specialising in functional imaging of the human body, and Marat, a doctor specialising in critical care medicine, exemplify the collaborative nature of biomedical engineering research and medical imaging.
Ting’s expertise in medical imaging was crucial for developing VINCI, because imaging techniques are used to measure how well blood is flowing through the brain during treatment and to check if the brain’s blood vessels are intact. “These imaging results provide us with detailed insights into the brain’s health during cooling, offering much more information than standard measurements like blood pressure, heart rate and pressure within the brain,” he explains. On the other hand, Marat’s role brings invaluable clinical perspectives to the project. His expertise informs the development of VINCI from a clinical usability standpoint and guides the design of clinical trial protocols. “This collaboration is important from the outset, as clinical constraints and realities inform the design and specifications of the developed device,” he explains.
The development of VINCI for stroke treatment is a great example of how biomedical engineering thrives on collaboration. “Developing and testing VINCI requires expertise in several areas: biomedical engineering to design and manage the technology, understanding of stroke pathophysiology to know how strokes affect the body and how to use medical imaging to monitor the treatment effects, and knowledge of clinical trial research to properly test VINCI’s effectiveness,” explains Ting. “It is also crucial to follow strict ethical standards during testing on both animals and humans to ensure that the results are not only reliable but also ethically obtained, providing meaningful and trustworthy outcomes.”
Pathway from school to biomedical engineering
To pursue a career in biomedical engineering or medical imaging, you should focus on building a strong foundation in mathematics, physics and biology at school and beyond.
At university, a degree in physics, biomedical engineering, another field of engineering (e.g., electronics), medicine, biomedical science, physiology or computer science could lead to a career in biomedical engineering.
Explore careers in biomedical engineering
Biomedical engineers develop engineering solutions to medical problems, so you could find yourself creating new hospital equipment, such as improved medical imaging tools, or building new medical devices, such as pacemakers and prosthetic limbs.
TRYEngineering (https://tryengineering.org/tag/biomedical-engineering/) has a wealth of information about biomedical engineering, including what biomedical engineers do, how to embark on a biomedical engineering educational and career pathway, and employment opportunities.
The Schulich School of Medicine & Dentistry at Western University runs the Experiential Learning Academy for Biomedical Sciences (X-LABS; www.schulich.uwo.ca/about/news/2023/july/xlabs-camp.html), which exposes local high school students to biomedical engineering by allowing them to participate in lab research and observe state-of-the-art demonstrations.
Meet Ting
What inspired you to become a biomedical engineer?
I’ve always been fascinated by how things work, which drew me to the interconnected worlds of physics and mathematics. However, I found physics to be somewhat abstract and not always directly linked to solving real-world problems, especially in biology and medicine. This curiosity led me to explore biomedical engineering, particularly the field of medical imaging. Here, the principles of physics and math merge in exciting ways, helping us see inside the human body without surgery.
Why does your research involve both theoretical and experimental work?
I’m drawn to the role of a theoretical scientist, where I build models that attempt to explain how things work. These models need to be tested through experiments to see if they truly hold up, bridging the gap between theory and practice. This process is crucial as it not only validates the models but also spurs further development and deepens our understanding of human biology, both in states of health and disease.
What motivated you to focus your research on brain cooling for improving stroke outcomes?
I’ve always been frustrated by the limitations of medical imaging. While it’s amazing that we can use imaging to detect diseases inside the body and response to treatment, it’s been a challenge that we can’t immediately treat what we see. My goal has been to achieve ‘theranostics’ – a blend of therapy and diagnostics where we can treat conditions as soon as we detect them and then verify the results through further imaging.
What do you enjoy doing in your free time?
I love reading because it takes me on incredible journeys through my imagination. My favourite books are about history and the lives of historical figures, especially scientists like Einstein, Tesla and Heisenberg.
Ting’s top tips
1. There are no shortcuts in science. Every scientific pursuit demands dedication and a lot of patience.
2. Keep an open mind and keep expanding your knowledge and skills. Scientific breakthroughs tend to occur unexpectedly, so you need to be ready to seize opportunities.
Meet Marat
Who inspired you to become a doctor?
My grandmother was a botanist, so I became interested in plants as a child, and my dad was a doctor, so I spent a lot of time at the hospital as my mother (a journalist) was away a lot. I loved science, but I became very interested in the art side of medicine, especially the patient-physician relationship that is central to the practice of medicine.
What does your role as an intensive care consultant involve?
I lead an interdisciplinary team of staff and learners, providing clinical care for the sickest patients in the hospital. This includes doing daily rounds, assessing patients, developing complex and comprehensive treatment plans, consulting with other experts (e.g., surgeons and infectious disease specialists), meeting with patients and their families, and providing end-of-life care to those patients who need it.
What are the highlights of your career?
As a young master’s student, I had the privilege to participate in research expeditions in Kazakhstan, Ethiopia, India and Bolivia to study the effects of altitude on cerebral blood flow. During these high-altitude expeditions, we studied our own cerebral blood flow as we acclimatised to the altitude, and we studied native populations who live at high altitude and so have developed adaptations.
Now, as a clinician-scientist, one of my most treasured and interesting roles is as an organ donation specialist.
What do you enjoy doing in your free time?
I love adventure, travel and spending time with family and friends. I also enjoy playing rugby, and I have started to learn jiu jitsu.
Marat’s top tips
1. Embrace your life as an adventure. Travel and seek opportunities outside of your immediate surroundings because the more you explore and experience, the better informed your career choices will be.
2. Don’t get discouraged – there are people out there who are willing to help you as long as you remain driven and optimistic.
Do you have a question for Ting or Marat?
Write it in the comments box below and Ting or Marat will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)
Learn how other researchers at Western University are using biomedical imaging techniques to improve our understanding of strokes:
www.futurumcareers.com/how-can-new-biomedical-imaging-techniques-help-us-understand-strokes



0 Comments