Growing human liver cells ‘in a dish’
Reference
https://doi.org/10.33424/FUTURUM04
Dr Dave Hay, Professor of Tissue Engineering
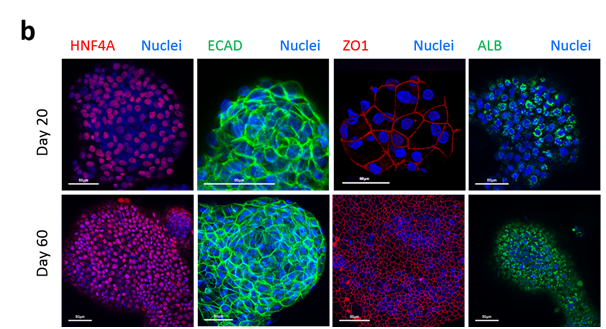
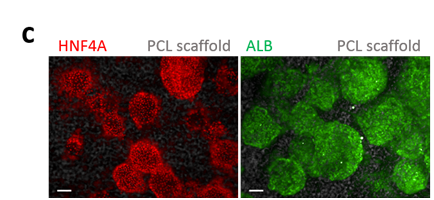
Evaluation of hepatic markers at gene and protein level. Photo courtesy of Dr Dave Hay
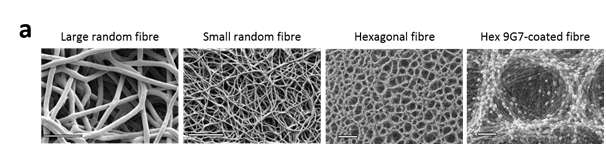
Development and characterisation of a sub-cutaneous implant. Photo courtesy of Dr Dave Hay
Development and characterisation of a sub-cutaneous implant. Photo courtesy of Dr Dave Hay
Full liver transplants are the main treatment option for severe liver disease, but suitable donors are in short supply. Could stem cell technology, in which healthy liver cells are grown in the lab, be a solution to this problem? Dr Dave Hay from the University of Edinburgh’s Centre for Regenerative Medicine thinks it could
A liver transplant involves removing a diseased liver and replacing it with a healthy one from a donor. While the operation may seem simple enough, it’s not without risks or complications. Dr Dave Hay from the Centre for Regenerative Medicine at the University of Edinburgh has been using stem cells to make new, healthy liver cells. He hopes that these new cells could be made into healthy liver tissue to replace damaged tissue in patients – an exciting prospect that could offer an alternative to liver transplants.
WHAT ARE STEM CELLS?
Stem cells are cells that are undifferentiated; that is, they don’t yet have a specific job or function. Under certain conditions, they take on their functions and become specific cells such as bone cells, fat cells or muscle cells. Pluripotent stem cells are those that can be grown into any type of tissue in the body.
It’s easy to see why, then, scientists have turned their attention to stem cell research. With stem cell technology, new cells of the needed type could be produced and used to replace damaged ones, and thus regenerate tissues and organs in patients.
WHAT DOES THE LIVER DO?
The liver is large reddish-brown organ that sits to the right side of the belly. Its job is to filter the blood coming from the digestive tract and to break down and remove unwanted materials. It also produces bile – a substance that helps the small intestine break down and absorb fats, cholesterol, and some vitamins. There are many other functions that the liver performs such as assisting the formation of blood clots, aiding with mineral storage, and supporting the immune system to fight disease, to name a few.
As you can imagine, liver damage is bad news for the body. The damage reduces the liver’s capacity to perform necessary functions. This negatively impacts a patient’s health, and can result in death. It’s vital, therefore, that liver disease is treated and that this is accompanied by the necessary lifestyle changes such as giving up or reducing alcohol intake, eating a balanced diet and exercising regularly.
HOW IS SEVERE LIVER DISEASE NORMALLY TREATED?
Some medications and surgical procedures may help. However, in cases of severe damage, a full liver transplant is the only option. The problem is, livers are in short supply. In some areas, suitable donors are unavailable. The shortfall
of suitable donors can also be worse for some patients depending on their ethnicity and the country in which they reside. Using stem cells to grow liver tissue in the lab, therefore, is seen as a possible solution to this problem.
HOW DO YOU MAKE NEW LIVER CELLS?
Making new cells in the lab is a complicated process. “In a nutshell,” Dave explains, “making new cells in the lab involves feeding the stem cells different factors and nutrients that are involved in human development”.
Depending on the conditions the stem cells are exposed to, scientists can make different types of cells, such as hepatocytes, the main cell type of the liver “Our interest is in the liver and, in particular, producing hepatocyte- like cells,” says Dave. “Our cells are similar to human adult liver cells but possess major foetal and neonatal attributes. So, we call them hepatocyte-like cells, and not hepatocytes, because they’re not fully mature.”
In the lab, Dave and his team use a material known as ‘agarose’ in which liver spheres form. Agarose is a material that is extracted from seaweed and used to make gels. These gels, when set, are the perfect growth medium. “Cells don’t bind to the agarose, meaning that they attach to each other and self-assemble into clumps,” says Dave. And it’s these clumps of new, healthy tissue that could be implanted into a patient in the future.
Reference
https://doi.org/10.33424/FUTURUM04
Dr Dave Hay, Professor of Tissue Engineering
Evaluation of hepatic markers at gene and protein level. Photo courtesy of Dr Dave Hay
Development and characterisation of a sub-cutaneous implant. Photo courtesy of Dr Dave Hay
Development and characterisation of a sub-cutaneous implant. Photo courtesy of Dr Dave Hay
A liver transplant involves removing a diseased liver and replacing it with a healthy one from a donor. While the operation may seem simple enough, it’s not without risks or complications. Dr Dave Hay from the Centre for Regenerative Medicine at the University of Edinburgh has been using stem cells to make new, healthy liver cells. He hopes that these new cells could be made into healthy liver tissue to replace damaged tissue in patients – an exciting prospect that could offer an alternative to liver transplants.
WHAT ARE STEM CELLS?
Stem cells are cells that are undifferentiated; that is, they don’t yet have a specific job or function. Under certain conditions, they take on their functions and become specific cells such as bone cells, fat cells or muscle cells. Pluripotent stem cells are those that can be grown into any type of tissue in the body.
It’s easy to see why, then, scientists have turned their attention to stem cell research. With stem cell technology, new cells of the needed type could be produced and used to replace damaged ones, and thus regenerate tissues and organs in patients.
WHAT DOES THE LIVER DO?
The liver is large reddish-brown organ that sits to the right side of the belly. Its job is to filter the blood coming from the digestive tract and to break down and remove unwanted materials. It also produces bile – a substance that helps the small intestine break down and absorb fats, cholesterol, and some vitamins. There are many other functions that the liver performs such as assisting the formation of blood clots, aiding with mineral storage, and supporting the immune system to fight disease, to name a few.
As you can imagine, liver damage is bad news for the body. The damage reduces the liver’s capacity to perform necessary functions. This negatively impacts a patient’s health, and can result in death. It’s vital, therefore, that liver disease is treated and that this is accompanied by the necessary lifestyle changes such as giving up or reducing alcohol intake, eating a balanced diet and exercising regularly.
HOW IS SEVERE LIVER DISEASE NORMALLY TREATED?
Some medications and surgical procedures may help. However, in cases of severe damage, a full liver transplant is the only option. The problem is, livers are in short supply. In some areas, suitable donors are unavailable. The shortfall of suitable donors can also be worse for some patients depending on their ethnicity and the country in which they reside. Using stem cells to grow liver tissue in the lab, therefore, is seen as a possible solution to this problem.
HOW DO YOU MAKE NEW LIVER CELLS?
Making new cells in the lab is a complicated process. “In a nutshell,” Dave explains, “making new cells in the lab involves feeding the stem cells different factors and nutrients that are involved in human development”.
Depending on the conditions the stem cells are exposed to, scientists can make different types of cells, such as hepatocytes, the main cell type of the liver “Our interest is in the liver and, in particular, producing hepatocyte- like cells,” says Dave. “Our cells are similar to human adult liver cells but possess major foetal and neonatal attributes. So, we call them hepatocyte-like cells, and not hepatocytes, because they’re not fully mature.”
In the lab, Dave and his team use a material known as ‘agarose’ in which liver spheres form. Agarose is a material that is extracted from seaweed and used to make gels. These gels, when set, are the perfect growth medium. “Cells don’t bind to the agarose, meaning that they attach to each other and self-assemble into clumps,” says Dave. And it’s these clumps of new, healthy tissue that could be implanted into a patient in the future.
HOW LONG WILL IT BE BEFORE LAB-GROWN LIVERS ARE USED TO TREAT PATIENTS?
Research by Dave and his team has found that their specially-designed liver tissue implants supported liver function in mice with a certain type of liver disease – an advance that could be the first step towards developing liver tissue implants for people.
For now, the researchers are focusing on being able to transplant small fragments of liver tissue into a patient until a suitable donor organ becomes available for transplant (rather than growing a full human liver). And the team are in the process of working with industry and writing grants to move towards this. Reflecting on current progress, Dave commented, “What I can say is this – we have a stable and renewable product we can apply to study human liver biology in the lab and hopefully one day use in the clinic.”
But, before any new therapy or intervention can be used on people, scientists have to show that that their work could become a reality – a process known as proof of concept – and conduct clinical trials. Dave hopes to have this proof of concept within the next five years.

DR DAVE HAY
Professor of Tissue Engineering
Centre for Regenerative Medicine
University of Edinburgh, UK
FIELD OF RESEARCH: Regenerative medicine, tissue engineering and stem cell biology
RESEARCH PROJECT: Dave’s research focuses on using stem cells to engineer tissue types and organs in the lab. For example, he has been working with pluripotent stem cells to create liver cells and tissue, with the goal of developing alternative treatment options to full liver transplants.
Funders: UK Regenerative Medicine Platform; Chief Scientist Office of Scotland
ASK DAVE
WHAT DID YOU WANT TO BE WHEN YOU WERE YOUNGER?
Initially, a footballer. The problem was, I wasn’t very good at it! But I always enjoyed biology and chemistry at school, and this led me to study biochemistry at university.
ACCORDING TO WILLIS TOWERS WATSON, MORE THAN 60% OF CHILDREN ATTENDING SCHOOL TODAY WILL WORK IN A CAREER THAT DOES NOT CURRENTLY EXIST. WOULD YOU SAY YOU’VE HAD A SIMILAR EXPERIENCE, I.E WORKING IN A REVOLUTIONARY FIELD THAT MAY NOT HAVE BEEN PARTICULARLY MAINSTREAM WHEN YOU WERE GROWING UP?
The isolation and reprogramming of human pluripotent stem cells had not been achieved until 1998 and 2007, respectively, so human pluripotent stem cell research was not mainstream until I was in my late 20s. So, yes, I definitely experienced that.
WHAT DO YOU LOVE MOST ABOUT YOUR WORK?
My job is great as it’s never the same each day. It includes supervising students, giving international presentations, examining experimental results, writing papers and grants, setting up companies…. There’s always something to be done! In science and grant writing there’s an element of trial and error, and taking criticism. The secret is not to become down about what people perceive as failure; rather to use any feedback you receive to reshape your thoughts and deliver success in the future.
HOW WOULD YOU DESCRIBE YOURSELF? ARE THESE CHARACTERISTICS/PERSONALITY TRAITS USEFUL IN A CAREER LIKE YOURS?
I’m hard working and determined. I think these are very important for a scientific career, as well as others. But it’s not all work; I enjoy spending time with my family, going on holiday to warm places, working out in the gym, good food and going out! Balance is also very important.
WHAT ADVICE WOULD YOU GIVE TO YOUNG PEOPLE WHO ARE STARTING OUT ON THEIR CAREER PATH, BUT AREN’T SURE ABOUT WHAT THEY’D LIKE TO DO IN THE FUTURE?
My advice would be to follow what interests you most. In this way you’ll not feel like you’re just working to an end. Rather, you’ll feel like you’re following your curiosity. This will make you more motivated.
ABOUT TISSUE ENGINEERING
Tissue engineering is an exciting field of study and many scientists and medical professionals feel it has great potential to treat numerous diseases. We ask Dave to tell us more about it.
WHAT IS TISSUE ENGINEERING AND HOW DOES IT FIT WITHIN THE WIDER CONTEXT OF STEM CELL RESEARCH AND REGENERATIVE MEDICINE?
Tissue engineering is the field of research that combines cells with biologic and synthetic components to build functional units of tissue. This allows the researcher to study tissue assembly, function, health and disease ‘in the dish’. It may also be later deployed within clinical setting to treat loss of function or disease.
IS REGENERATIVE MEDICINE BEING USED IN HOSPITALS NOW?
Yes, bone marrow transplant is a good example of stem cell therapy. With regard to pluripotent stem cell-derived therapies, they have been used clinically to successfully correct macular degeneration and will be used this year in trials aimed at treating Parkinson’s disease.
IF RESEARCH SUCH AS YOURS WON’T BE IN EVERYDAY USE FOR SO MANY YEARS, WHY GET EXCITED ABOUT IT?
Our ability to make human tissue from any individual – subject to consent and ethics processes – enables us to study their characteristics ‘in a dish’. This allows us to better understand disease and tailor make treatments for that disease. That’s exciting because the technology will provide us with great opportunities to treat tissue damage and degenerative diseases. These technologies will transform medicine as we move through the next 10-20 years.
OTHER THAN GOING TO UNIVERSITY, ARE THERE OTHER ROUTES TO WORKING IN STEM CELL RESEARCH OR REGENERATIVE MEDICINE?
Yes, regenerative medicine is a broad field, spanning many disciplines. Therefore, a number of routes are available. For example, you could work in administration, technical assistance, quality control, facilities maintenance and project management. This could be within an established company or a start-up company.
WOULD YOU RECOMMEND REGENERATIVE MEDICINE AS A REWARDING CAREER OPTION FOR YOUNG PEOPLE?
I really enjoy my job. It has its challenges, but these are outweighed by its rewards!
OPPORTUNITIES IN BIOMEDICAL ENGINEERING
- Tissue engineering is a highly specialised field of research, so it will require a bachelor’s degree in biology or related fields, and then postgraduate qualifications in biomedical engineering. Check with your local university to see what options are available to you.
- Another option, if you would like to see if working in biomedicine or a clinical setting is for you, is to do a course in medical laboratory technology. Technical training centres offer suchlike courses.
- In the UK, biomedical engineers earn between £21,000 and £45,000.

An excellent informative article published in a very readable format. I have printed off all 14 pages for future reference.
Well done Professor Hay.
Hello,
Have you successfully transplanted stem cells to be used as liver cells into human?
Many thanks for your question Mare. We are working toward human trails. Before this is possible we are testing graft safety, the optimal dose and long term performance in the appropriate pre-clinical models.