How can health and care support break the cycle of homelessness?
People experiencing homelessness often face significant health and well-being challenges, but accessing health and care support can be very difficult for them. Dr Michela Tinelli, a health and care economist at the London School of Economics and Political Science in the UK, is investigating how out-of-hospital care models can provide more meaningful care for people experiencing homelessness. Her research is contributing to data-driven decision-making that will improve these services.
Talk like a health and care economist
Data science — the collection and analysis of data to extract meaningful insights
Discrete choice experiment — a quantitative research method for understanding people’s preferences and decision-making processes, in which participants are asked to choose between hypothetical choices
Integrated management dashboard — an interactive platform that allows a user to visualise a range of datasets and extract meaningful insights
Out-of-hospital care model — any type of care not undertaken in a hospital setting
Stakeholder — anyone who uses (e.g., patients, carers), provides (e.g., healthcare professionals, social workers) or commissions (e.g., local authorities, government departments) a service
Step-down services — services for patients discharged from hospitals, typically integrating health and social care needs
“People experiencing homelessness commonly face a range of health and social challenges,” says Dr Michela Tinelli, a health and care economist at the London School of Economics and Political Science. “For instance, exposure to the elements during rough sleeping results in increased vulnerability to illness.” The stress of living on the streets, coupled with social isolation and discrimination, means that people experiencing homelessness are also vulnerable to mental health problems. Homelessness makes it much harder to access healthcare, education and employment opportunities, which compounds these problems. This highlights the need for services that address these issues.
“People experiencing homelessness need access to healthcare and mental health services, community clinics focused on the needs of the homeless population, and services to connect individuals with housing and employment opportunities,” says Michela. Out-of-hospital care models play a crucial role in providing these services, and Michela is exploring how to optimise these models to provide the best possible care.
Out-of-hospital care models
Out-of-hospital care models provide health and social care services in the community, rather than in hospitals. For example, step-down services address the unique needs of people without stable housing by providing transitional care facilities for people leaving hospital. Often, if a person experiencing homelessness is discharged from hospital with no further follow-up, they will remain homeless. Step-down services aim to address this. “The primary goal of step-down services is to provide individuals with a supportive environment that promotes recovery and stability,” explains Michela. “This approach recognises the interconnectedness of healthcare and social factors for improving well-being and quality of life.”
The importance of data science
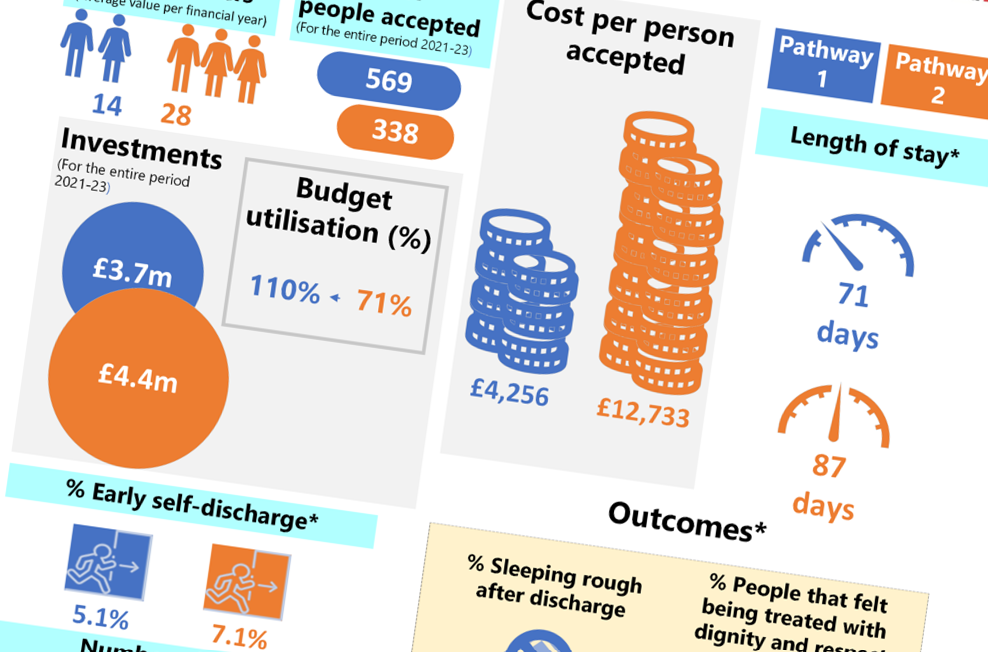
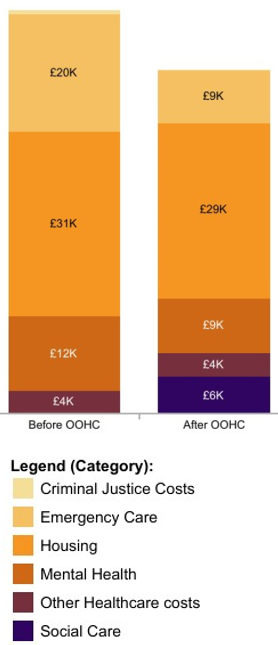
Michela and her team used a mixture of qualitative and quantitative methods to evaluate out-of-hospital care models used in England. “We conducted qualitative interviews with people experiencing homelessness, healthcare professionals and other out-of-hospital care model stakeholders,” she says. “These discussions allowed for in-depth exploration of personal experiences of and insights into the services.” Quantitative methods included surveys of participants’ experiences and analyses of outcomes (such as rates of readmission to hospital or return to homelessness) and service delivery costs.
Michela also used discrete choice experiments to understand what people experiencing homelessness want from out-of-hospital care models. These surveys asked participants to choose between two hypothetical situations, to understand their preferences and what trade-offs are acceptable for them. “For example, we asked how long people would be willing to wait to receive care in their own home, compared to receiving care immediately in temporary accommodation,” explains Michela. Data science methods such as these will help to inform the rollout of services that cater directly to the needs of the community. For instance, the discrete choice experiments uncovered some interesting results. “Unsurprisingly, participants strongly expressed their aversion to returning to rough sleeping, compared to accessing step-down services,” says Michela. “By synthesising their preferences, we deduced that the ideal care service model encompasses a housing support worker visiting the participant’s own accommodation three to four times a week, for a duration of ten to twelve weeks.” Crucially, this suggests that a stable, private living arrangement – having their own flat, rather than living temporarily in a hostel – makes people experiencing homelessness more likely to access health and social care services.
Michela’s results suggest the impacts of out-of-hospital care models are strongly positive. “We collected data from 1,254 homeless patients, many of whom experienced improvements in quality of life and felt they were treated with dignity and respect through these services,” says Michela. “Only 7% returned to rough sleeping after accessing step-down services, compared to around 77% before these services existed.”
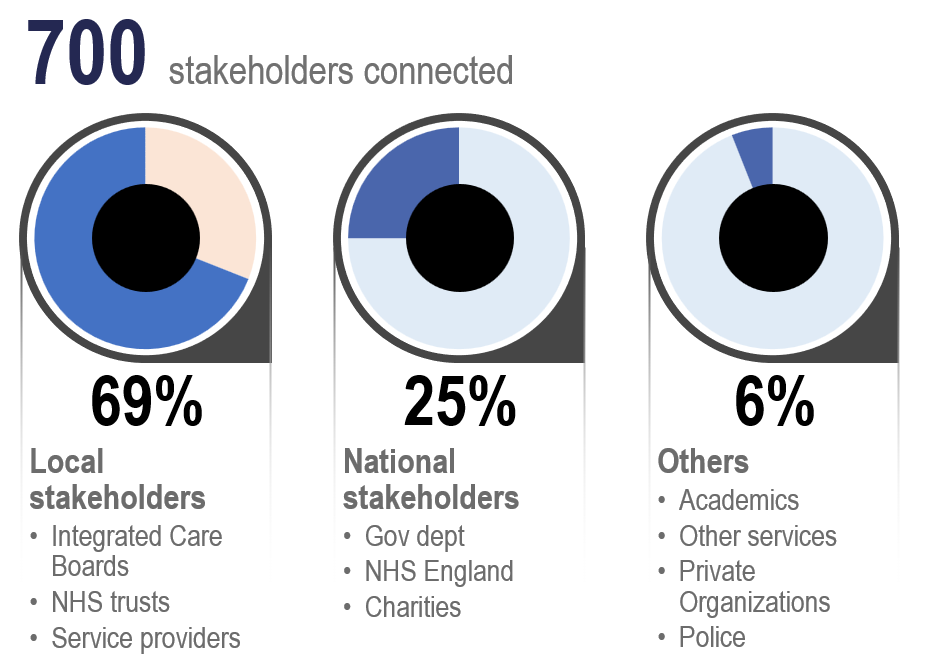
Developing dashboards
Using the insights gathered from her results, Michela developed integrated management dashboards to serve as tools for out-of-hospital care model stakeholders. “The objectives of these dashboards include monitoring the performance of out-of-hospital care models, assessing the quality of care received by patients and optimising the allocation of resources,” says Michela. The interactive dashboards allow users to visualise data through clear and customisable presentations. “They empower the monitoring and evaluation of current events, allowing for immediate action based on present insights (what is happening now) instead of relying on published reports with outdated data (what happened in the past),” she explains. “The dashboards provide actionable insights for stakeholders. They facilitate data-driven decision-making to enhance the effectiveness of out-of-hospital care for people experiencing homelessness.”
There is strong support for the integrated management dashboards as operational and management tools. Stakeholders report they are useful for enhancing evidence-based decision-making. Michela is now in conversation with local health and care providers around England to provide the dashboards to out-of-hospital care model stakeholders throughout the country.
From research to policy
Thanks to the data science research of health and care economists such as Michela, services and national policies will improve the health outcomes for people experiencing homelessness. “Our analysis offers practical guidance for policy development,” says Michela. “It informs policymakers where to focus their efforts and resources to align with the preferences of those accessing and implementing these services.” Furthermore, these results will help to optimise out-of-hospital care model services, improving quality of care and tailoring support to those in need. “Our outputs will support decision-making for the health and well-being of the population at the national level.”
Reference
https://doi.org/10.33424/FUTURUM471
 Dr Michela Tinelli
Dr Michela Tinelli
Care Policy and Evaluation Centre, London School of Economics and Political Science, UK
Fields of research: Health and care economics, evaluation, social care
Research project: Developing management resources to optimise out-of-hospital care models for people experiencing homelessness
Funders: UK Department of Health and Social Care (DHSC), National Institute for Health and Care Research – School for Social Care Research (NIHR SSCR)
Michela Tinelli (LSE) and Michelle Cornes (King’s College London and Salford University) co-led the national programme of out-of-hospital care models for people who are homeless. The evaluation was funded by DHSC and the full team is acknowledged here. Michela was awarded a Developing Research Leadership Fellowship by NIHR SSCR to apply the discrete choice experiment technique to social care.
About health and care economics
The field of health and care economics investigates how to allocate health and care resources in the most effective way possible. Michela explains more about her field:
“Health and care economists investigate the allocation, distribution and utilisation of resources in healthcare systems. They aim to understand the economic aspects of health and care delivery, alongside the impacts of health policies and interventions. Health and care economists may investigate different models of healthcare financing or evaluate the cost-effectiveness of healthcare interventions.
“Researchers in my field contribute to shaping decisions that directly impact people’s well-being. The field tackles pressing societal issues, including healthcare accessibility, affordability and the equitable distribution of resources. Working in the field is very rewarding as it provides opportunities to make meaningful and positive differences in people’s lives. My job satisfaction comes from knowing that my work directly aligns with societal well-being and the improvement of healthcare systems.
“Health and care economics draws on insights from economics, public health, policy analysis, data science and social sciences. This interdisciplinary approach provides a dynamic and diverse work environment, and addressing health and social care challenges requires collaboration among many stakeholders. This includes researchers, healthcare professionals, policymakers, community organisations and individuals. Together, we can inspire a commitment to collective solutions.”
Pathway from school to health and care economics
At school and beyond, Michela recommends studying mathematics (especially statistics), economics, biology or health sciences, and psychology to gain quantitative and data analysis skills and to learn about human health and behaviour.
At university, a degree in economics, public health or public policy could lead to a career in health and care economics. Michela recommends taking classes in health economics, econometrics, statistics, health policy analysis, health services management, global health and ethics in healthcare.
Explore careers in health and care economics
Health and care economists may work as researchers for universities, governments or healthcare organisations, or they may apply their work as policymakers to improve health and social care.
Michela recommends seeking internships or work experience in healthcare organisations, research institutions or government agencies. “This opportunity will allow you to make a meaningful contribution towards their work, while preparing for your GCSEs or A levels,” she says. Talk to your school careers adviser about the possibility of work experience. You can send your CV to Michela ([email protected]) if you are interested in gaining hands-on experience with her team or working with the Care Policy and Evaluation Centre at the London School of Economics and Political Science (www.lse.ac.uk/cpec).
Meet Michela
I’ve always had a curiosity for mathematics, economics and health science, which laid the foundation for my interest in health and care economics. Growing up, an awareness of societal issues and a concern for the well-being of others manifested in a desire to improve the delivery of healthcare. Early experiences in college sparked a passion for research and knowledge creation – I wanted to create something new that nobody else had done before.
I originally studied pharmacy and spent time working as a pharmacist (both in a lab and as a community pharmacist). Pharmacy offers the opportunity to directly improve people’s health and well-being by providing medication-related expertise. The scientific aspects of pharmacy, such as the effects of pharmaceuticals on the human body, aligned with my interests in chemistry, biology, and how genetic engineering can optimise the production of pharmaceutical compounds.
I soon switched from pharmacy lab work to applied research (in health and care) because I was deeply passionate about improving healthcare systems. I wanted to make a concrete positive impact on public health by addressing societal challenges. I wanted to connect with different stakeholders to help them optimise services and gain better outcomes for patients and society.
My mum, husband and daughter all suffer from asthma, and their health issues inspire me to make positive changes to healthcare systems. I believe that better health and care services must be tailored to the needs and preferences of individuals. More broadly, my passion for health and care economics is rooted in genuine concern for the well-being of communities and society as a whole.
My hobbies depend on the season. I enjoy ice skating in winter, wakeboarding in the summer, and cooking all year round!
Michela’s top tips
Be passionate about what you do, keep going even when it’s tough, be open to new ideas and opportunities, and always have fun!
Do you have a question for Michela?
Write it in the comments box below and Michela will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)
3 Comments
Submit a Comment
Learn how health economists are improving the effectiveness of medical trials:
www.futurumcareers.com/how-can-we-improve-the-cost-effectiveness-of-medical-trials








Hi, im currently looking forward to pursue my PHD and interested in investigating on how to improve public health record across hospital to enhance the treatment receive by the patient and to improve service delivery in public hospital. My background is in accounting field; particularly dealing with management accounting and decision making process.
Hi Nur,
Thanks for writing in. It sounds like you have an exciting journey ahead. It’s great that you’re able to bring a diverse skill set to work on improving patient experiences and service delivery in healthcare settings. We wish you all the best with your PhD.
Futurum Webmaster
Hi Michele,
Can I just say thank you for you. I’m conscious of posting on such a public profile and hope we might be able to continue a conversation by email?
Thanks in Advance
Danielle & Wolfie 🐾