How can we treat multidrug-resistant tuberculosis?
TALK LIKE AN EPIDEMIOLOGIST
TUBERCULOSIS (TB) – an infectious bacterial disease that most commonly affects the lungs but can affect any part of the body
DRUG RESISTANCE – the ability of disease-producing pathogens to survive the effects of drugs that would usually kill them
EFFICACY – the ability of a drug to produce the desired effect in a clinical trial setting
EFFECTIVENESS – the extent to which a drug is effective under real-world conditions
ADHERENCE – the degree to which a patient follows the treatment regimen prescribed to them by a healthcare professional
ADVERSE EFFECTS – unexpected medical problems that occur whilst a patient is receiving treatment
REPRODUCIBILITY – the ability to produce the same results if a study or experiment is repeated
GENERALISABILITY – the extent to which findings from a study can be applied to other settings
SUPERIORITY TRIAL – a randomised trial designed to assess whether a new treatment or intervention is more effective than another
NON-INFERIORITY TRIAL – a randomised trial designed to assess whether a new treatment or intervention is not much worse when compared to a standard treatment or care
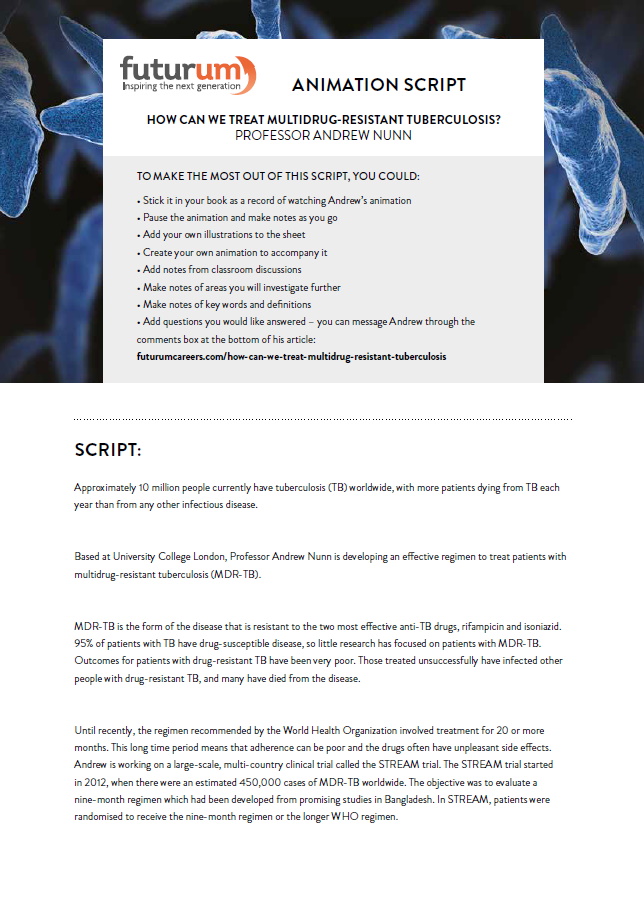
It is estimated that approximately 10 million people currently have tuberculosis (TB) worldwide, with more patients dying from TB each year than from any other infectious disease. Approximately 5% of people with TB have a form of the disease that is resistant to rifampicin, one of the most effective and commonly used drugs used for treatment. Most of these patients also have resistance to isoniazid, another important drug used for treating TB. Based at University College London, Professor Andrew Nunn’s research aims to develop an effective regimen to treat patients with drug-resistant TB and thereby reduce its spread. Before the 1970s, treatment of tuberculosis involved a course of at least three drugs given for a minimum of 18 months. “The results under programme conditions were often poor due to adverse effects and poor adherence to treatment,” explains Andrew.
In the mid-1960s, a new drug called rifampicin was discovered. “Results from laboratory studies were very promising and the research group I was working with proposed a radical departure from standard treatment, treating patients for only six months with a rifampicin-containing regimen,” he says. After positive results in a series of trials, this treatment became standard throughout the world.
MULTIDRUG-RESISTANT TUBERCULOSIS
However, not all patients were treated successfully on this new regimen. Some treatments failed due to poor adherence and resistance developed to drugs in the regimen. Over time, people with drug-resistant TB infected people they were in contact with, adding to the number of patients with drug-resistant TB. Multidrug-resistant tuberculosis (MDR-TB) is the name given to the form of TB that is resistant to the two most effective anti-TB drugs, rifampicin and isoniazid.
Studies conducted in the 1970s and 80s showed that patients with no evidence of drug resistance could be treated effectively with the six-month regimen, provided they adhered to treatment. However, those with rifampicin resistance had poor outcomes, even if they had no evidence of resistance to any other drugs. “Because 95% of patients with TB have drug-susceptible disease, for many years the focus of research was on this very large patient group. Little attention was paid to patients with rifampicin-resistant TB,” explains Andrew.
TREATMENT
The World Health Organization (WHO) collects information on the number of TB cases and treatment outcomes in each country on an annual basis. “For many years, these results have shown that outcomes for patients with rifampicin-resistant TB were very poor, only about 50% achieving a cure or even completing their treatment,” says Andrew. Often, those treated unsuccessfully went on to infect other people with rifampicin-resistant TB, and many died from their disease. As drug-resistant TB remains ineffectively treated, its spread accelerates and affects an increasing number of people.
“Unlike a disease like HIV, there has not been a sustained programme of research to develop new drugs for TB,” explains Andrew. The development of TB drugs has been very slow – it took 50 years between the discovery of rifampicin and the licensing of the next new TB drug. “The main reason for this is that TB is predominantly, although by no means exclusively, a disease affecting low- and middle-income countries,” adds Andrew.
For patients with rifampicin-resistant TB, the treatment options are even more limited. Until recently, the regimen recommended by the WHO involved treatment for 20 or more months. “Adherence to long regimens is poor and the drugs often have unpleasant side effects which further reduces the effectiveness of the regimen,” explains Andrew.
NEW REGIMENS
Much of Andrew’s work involves a large-scale, multi-country clinical trial called the STREAM trial (The Evaluation of a Standard Treatment Regimen of Anti-Tuberculosis Drugs for Patients with MDR-TB). The STREAM trial started in 2012 with the objective of evaluating a nine-month regimen which had been developed from a series of cohort studies conducted in Bangladesh and had shown very promising results. Although this regimen had the potential to be a considerable improvement on the WHO-recommended regimen, it had not been assessed in a randomised trial and there were concerns about its reproducibility and generalisability.
In STREAM, patients were randomised to receive the nine-month regimen or the longer WHO regimen. At the time the trial was started in 2012, there were an estimated 450,000 cases of MDR-TB worldwide. Less than a quarter of these were estimated to have been detected, and fewer still treated.
Clinical trials in TB often build on the work of previous studies, as in the case of STREAM. The process can take a long time due to the length of the treatment regimen and the need to follow patients after treatment has been completed to establish whether those who are cured remain disease free and do not relapse and need retreatment. To assess whether results are generalisable, they need to be conducted in a variety of settings.
SELECTING DRUGS FOR THE REGIMEN
“The nine-month regimens used in the STREAM trial and the Bangladesh study target maximum effectiveness rather than efficacy,” explains Andrew. Some drugs considered to have reasonable efficacy may not be effective in real world settings because they are known to be toxic or poorly tolerated; these were not included in the regimen. Doses were chosen to achieve maximum effectiveness. A higher than usual dose of moxifloxacin was used in this regimen to assist in preventing further drug-resistance. As moxifloxacin is known to increase the risk of QT prolongation, a heart rhythm condition that can potentially lead to fainting, palpitations, and, in exceptional cases, sudden death, safety monitoring for QT prolongation was done as part of the trial. Clofazimine, a drug that had been more often used for treating leprosy than TB, was included in the regimen as it had shown potential in laboratory studies.
Reference
https://doi.org/10.33424/FUTURUM216
TUBERCULOSIS (TB) – an infectious bacterial disease that most commonly affects the lungs but can affect any part of the body
DRUG RESISTANCE – the ability of disease-producing pathogens to survive the effects of drugs that would usually kill them
EFFICACY – the ability of a drug to produce the desired effect in a clinical trial setting
EFFECTIVENESS – the extent to which a drug is effective under real-world conditions
ADHERENCE – the degree to which a patient follows the treatment regimen prescribed to them by a healthcare professional
ADVERSE EFFECTS – unexpected medical problems that occur whilst a patient is receiving treatment
REPRODUCIBILITY – the ability to produce the same results if a study or experiment is repeated
GENERALISABILITY – the extent to which findings from a study can be applied to other settings
SUPERIORITY TRIAL – a randomised trial designed to assess whether a new treatment or intervention is more effective than another
NON-INFERIORITY TRIAL – a randomised trial designed to assess whether a new treatment or intervention is not much worse when compared to a standard treatment or care
It is estimated that approximately 10 million people currently have tuberculosis (TB) worldwide, with more patients dying from TB each year than from any other infectious disease. Approximately 5% of people with TB have a form of the disease that is resistant to rifampicin, one of the most effective and commonly used drugs used for treatment. Most of these patients also have resistance to isoniazid, another important drug used for treating TB. Based at University College London, Professor Andrew Nunn’s research aims to develop an effective regimen to treat patients with drug-resistant TB and thereby reduce its spread. Before the 1970s, treatment of tuberculosis involved a course of at least three drugs given for a minimum of 18 months. “The results under programme conditions were often poor due to adverse effects and poor adherence to treatment,” explains Andrew.
In the mid-1960s, a new drug called rifampicin was discovered. “Results from laboratory studies were very promising and the research group I was working with proposed a radical departure from standard treatment, treating patients for only six months with a rifampicin-containing regimen,” he says. After positive results in a series of trials, this treatment became standard throughout the world.
MULTIDRUG-RESISTANT TUBERCULOSIS
However, not all patients were treated successfully on this new regimen. Some treatments failed due to poor adherence and resistance developed to drugs in the regimen. Over time, people with drug-resistant TB infected people they were in contact with, adding to the number of patients with drug-resistant TB. Multidrug-resistant tuberculosis (MDR-TB) is the name given to the form of TB that is resistant to the two most effective anti-TB drugs, rifampicin and isoniazid.
Studies conducted in the 1970s and 80s showed that patients with no evidence of drug resistance could be treated effectively with the six-month regimen, provided they adhered to treatment. However, those with rifampicin resistance had poor outcomes, even if they had no evidence of resistance to any other drugs. “Because 95% of patients with TB have drug-susceptible disease, for many years the focus of research was on this very large patient group. Little attention was paid to patients with rifampicin-resistant TB,” explains Andrew.
TREATMENT
The World Health Organization (WHO) collects information on the number of TB cases and treatment outcomes in each country on an annual basis. “For many years, these results have shown that outcomes for patients with rifampicin-resistant TB were very poor, only about 50% achieving a cure or even completing their treatment,” says Andrew. Often, those treated unsuccessfully went on to infect other people with rifampicin-resistant TB, and many died from their disease. As drug-resistant TB remains ineffectively treated, its spread accelerates and affects an increasing number of people.
“Unlike a disease like HIV, there has not been a sustained programme of research to develop new drugs for TB,” explains Andrew. The development of TB drugs has been very slow – it took 50 years between the discovery of rifampicin and the licensing of the next new TB drug. “The main reason for this is that TB is predominantly, although by no means exclusively, a disease affecting low- and middle-income countries,” adds Andrew.
For patients with rifampicin-resistant TB, the treatment options are even more limited. Until recently, the regimen recommended by the WHO involved treatment for 20 or more months. “Adherence to long regimens is poor and the drugs often have unpleasant side effects which further reduces the effectiveness of the regimen,” explains Andrew.
NEW REGIMENS
Much of Andrew’s work involves a large-scale, multi-country clinical trial called the STREAM trial (The Evaluation of a Standard Treatment Regimen of Anti-Tuberculosis Drugs for Patients with MDR-TB). The STREAM trial started in 2012 with the objective of evaluating a nine-month regimen which had been developed from a series of cohort studies conducted in Bangladesh and had shown very promising results. Although this regimen had the potential to be a considerable improvement on the WHO-recommended regimen, it had not been assessed in a randomised trial and there were concerns about its reproducibility and generalisability.
In STREAM, patients were randomised to receive the nine-month regimen or the longer WHO regimen. At the time the trial was started in 2012, there were an estimated 450,000 cases of MDR-TB worldwide. Less than a quarter of these were estimated to have been detected, and fewer still treated.
Clinical trials in TB often build on the work of previous studies, as in the case of STREAM. The process can take a long time due to the length of the treatment regimen and the need to follow patients after treatment has been completed to establish whether those who are cured remain disease free and do not relapse and need retreatment. To assess whether results are generalisable, they need to be conducted in a variety of settings.
SELECTING DRUGS FOR THE REGIMEN
“The nine-month regimens used in the STREAM trial and the Bangladesh study target maximum effectiveness rather than efficacy,” explains Andrew. Some drugs considered to have reasonable efficacy may not be effective in real world settings because they are known to be toxic or poorly tolerated; these were not included in the regimen. Doses were chosen to achieve maximum effectiveness. A higher than usual dose of moxifloxacin was used in this regimen to assist in preventing further drug-resistance. As moxifloxacin is known to increase the risk of QT prolongation, a heart rhythm condition that can potentially lead to fainting, palpitations, and, in exceptional cases, sudden death, safety monitoring for QT prolongation was done as part of the trial. Clofazimine, a drug that had been more often used for treating leprosy than TB, was included in the regimen as it had shown potential in laboratory studies.
THE STREAM TRIAL
424 patients from seven sites in four countries – Ethiopia, Mongolia, Vietnam and South Africa – were enrolled in the first stage of the trial. Patients had to attend the study clinic every four weeks for two and a half years for treatment and follow-up appointments. Sputum samples were collected on each occasion to assess for possible treatment failure or relapse. The outcome of treatment was classed as unfavourable if they were not cured, they relapsed, had to change their allocated regimen, were lost to follow-up or died from any cause.
THE RESULTS SO FAR
STREAM was a non-inferiority trial, meaning that the aim was to check that the new regimen was not much worse than the existing treatment. The difference in the proportion of favourable outcomes between the control regimen (the 20 month WHO-recommended regimen) and the nine-month study regimen was calculated. Although the long WHO regimen had a 1.0% higher success rate, this difference and the confidence interval around the difference was small enough for the new regimen to be considered to be non-inferior. The proportion of severe adverse effects was very similar in the two regimens. “These results confirmed that the regimen studied in Bangladesh is effective in a variety of settings including countries like South Africa where there is a high level of HIV-TB coinfection,” explains Andrew.
WHAT’S NEXT?
Following the initial results of the STREAM trial, the majority of TB programmes are moving away from the long WHO regimen. The WHO will continue to revise its recommendations as new results become available. “The second stage of STREAM is evaluating a fully oral regimen (where there is no need for injections) and a six-month regimen. It is hoped that, ultimately, regimens of less than six months will be available for all patients with TB,” says Andrew.
STREAM is the first multi-centre randomised trial in MDR-TB and the results have been impressive. Over recent decades, Andrew, and researchers like him in the field of epidemiology, have shown that life-changing progress can be made in effective treatments and patient care through well-conducted clinical trials.
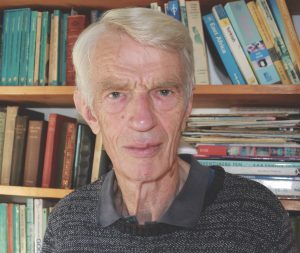 PROFESSOR ANDREW NUNN
PROFESSOR ANDREW NUNN
MRC Clinical Trials Unit, University College London, UK
FIELD OF RESEARCH: Epidemiology, Clinical Trials
RESEARCH PROJECT: Improving the effectiveness of treatment for tuberculosis patients who have resistance to the major drugs usually used to treat the disease
FUNDER: Medical Research Council, University College London
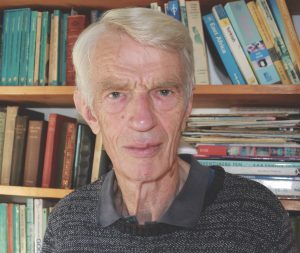 PROFESSOR ANDREW NUNN
PROFESSOR ANDREW NUNN
MRC Clinical Trials Unit, University College London, UK
FIELD OF RESEARCH: Epidemiology, Clinical Trials
RESEARCH PROJECT: Improving the effectiveness of treatment for tuberculosis patients who have resistance to the major drugs usually used to treat the disease
FUNDER: Medical Research Council, University College London
ABOUT EPIDEMIOLOGY
As an epidemiologist working on clinical trials, Andrew’s days are spent on a wide variety of activities, which may include developing ideas for new studies and study protocols, visiting the sites participating in his studies and discussing issues and progress of ongoing trials. A very important aspect of the work is presenting research findings at conferences and publishing results in peer-reviewed journals, in addition to researching the work of other scientists. Andrew also participates in oversight committees for trials being conducted by other research groups.
Epidemiologists work with scientists from diverse backgrounds to discover ways to improve healthcare. At the same time, they may also support colleagues to develop their skills. “I was privileged to be part of a research group based in Uganda from 1989-95 which provided very important insights into the dynamics of the HIV epidemic in that country,” says Andrew. The research programme was based in a poor rural community where many of those infected were young adults who were parents of young children. “At the time, very little was known about how HIV was transmitted in countries like Uganda and no effective treatment for HIV existed, even in the developed world,” explains Andrew.
“The coronavirus pandemic is a very good example of the challenges that face epidemiologists when a new disease emerges,” says Andrew. As different diseases continue to emerge, future epidemiologists will face fresh challenges as they work to understand the causes of new diseases and how diseases affect different population groups. It is then the job of epidemiologists to identify preventative and curative treatments for these diseases. “There is likely to be an increasing need for epidemiologists in the future,” says Andrew.
EXPLORE A CAREER IN EPIDEMIOLOGY
• The London School of Hygiene & Tropical Medicine has an excellent website, www.lshtm.ac.uk, highlighting a wide range of research activities.
• Watch or read the news and scientific journals, particularly those that are open access – such as BMJ Open, TRIALS and PLOS Medicine – to keep up to date with public health issues around the world.
• Volunteer with your local healthcare provider or public health charities to gain experience and understanding of how disease prevention works.
• Explore the work that organisations such as the World Health Organization and Centers for Disease Control and Prevention are involved in.
• The Medical Research Council Clinical Trials Unit provides work experience placements to A-level students via its In2Science programme.
• Visit science fairs such as the MRC Festival of Medical Research at University College London.
• According to Glassdoor, the average salary for people working in the field of epidemiology is £42,000.
• Andrew explains that epidemiology is a broad field; there are opportunities for those with either a clinical or mathematical background.
• Epidemiological research is very practical, providing opportunities for those with operational skills and interests.
• Subjects such as mathematics and statistics are key for epidemiologists. Biology, chemistry and human geography are also important.
• Attention to detail, critical thinking, clear communication, and knowledge and interest in health issues are important skills for aspiring epidemiologists.
HOW DID ANDREW BECOME AN EPIDEMIOLOGIST?
WHAT WERE YOUR INTERESTS WHEN YOU WERE GROWING UP? DID YOU ALWAYS LOVE MATHS AND SCIENCE?
Maths was my favourite subject at school, and I enjoyed books about maths. Although I didn’t study statistics at school, it always fascinated me. After completing a maths degree, which had a statistics module in it, I decided I wanted to learn more about statistics and enrolled on a master’s course. At that stage, I didn’t know that statistics could have such an important role to play in medicine.
WHAT WAS IT ABOUT MEDICAL RESEARCH THAT YOU FOUND SO INSPIRING?
I had no idea that a statistics degree could be an opening to medical research until, just before leaving university, the careers office suggested I should meet with Professor Sir Richard Doll. Professor Doll conducted the landmark study which conclusively demonstrated the link between smoking and lung cancer. I was excited to find that my qualifications could be used in such a worthwhile activity. What I have particularly enjoyed is delivering a well-conducted trial – it is even better when there is a positive result which will have an impact on the lives of patients, particularly in poor countries. From the start, I was excited by the prospect of doing a job that could benefit some of those most in need. I have absolutely no regrets about taking this career path and am extremely grateful to the advice I received from the careers office.
WHAT ATTRIBUTES HAVE MADE YOU SUCCESSFUL IN YOUR WORK?
I think the fact that I enjoy my job is a big factor. Attention to detail and recognising the importance of teamwork are also key.
HOW DO YOU OVERCOME OBSTACLES/SWITCH OFF FROM YOUR WORK?
I ask when I need help. This seems simple, but it’s a remarkably important thing to do. I enjoy cycling and gardening when I’m not working – this helps me to switch off and enjoy the outdoors.
WHAT ARE YOUR PROUDEST CAREER ACHIEVEMENTS?
Teamwork is an essential part of epidemiology and I am proud of having been able to work with some excellent scientists on important health projects. It was particularly exciting when we made the breakthrough to reduce tuberculosis treatment from 18 to 6 months in just one study. The HIV work in Uganda also stands out as a great collaboration with local Ugandans and international scientists.
ANDREW’S TOP TIPS
01 Ask yourself or a critical friend whether you have most of the following qualities: good at maths, attention to detail, the ability to think critically and to communicate clearly, an interest in health issues.
02 Look at epidemiology journals and introductory books on epidemiology and statistics.
03 Find events where you may be able to meet an epidemiologist or biostatistician to find out what they do. University open days may be a good place to start.
Do you have a question for Andrew?
Write it in the comments box below and Andrew will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)