How does pre-birth milk expression help with breastfeeding?
The benefits of breastfeeding newborn infants are long-established. However, the idea of expressing milk while pregnant, before the baby is born, is a relatively new one. At the University of Pittsburgh in the US, Dr Jill Demirci is researching why antenatal milk expression is becoming increasingly popular and whether this technique might improve breastfeeding post-birth.
TALK LIKE A NURSING SCIENTIST
Antenatal — before birth
Antibodies — proteins that protect you when an unwanted substance enters your body
Body mass index (BMI) — a measure of body fat based on height and weight
Colostrum — the first milk produced during pregnancy and the first days after birth that is low in total volume but high in antibodies
Hand expression — expressing breast milk by hand
Milk expression — removing milk from the breast by any method (e.g., electric breast pump, hand expression), so that it can be stored and fed to a baby later
Infant formula — nutrition for babies, which can be a substitute for breast milk; sold as a ready-to-feed liquid or a powder to be mixed with water
Postpartum — after childbirth
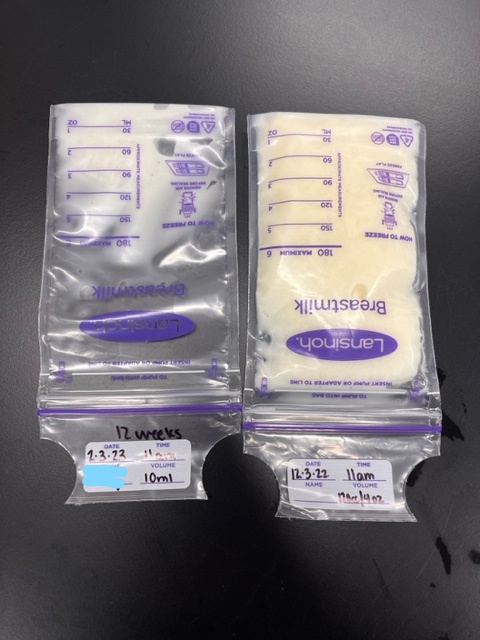
Antenatal milk expression, also known as AME, is becoming increasingly popular worldwide. It involves self-collecting early milk from the breasts, often around the 36-37th week of pregnancy (though it can be available earlier), which may then be frozen for a child to have once they are born.
“There are no major US-based maternal child health organisations recommending or not recommending AME,” says Dr Jill Demirci, a nursing scientist at the University of Pittsburgh. While not everyone chooses or is able to breastfeed, Jill notes that societal pressure to succeed at breastfeeding may cause parents to jump at the chance to get a head start though AME and increase their chances of successful breastfeeding. “They might hear about AME through other breastfeeding parents, health providers who have read the early research on AME or more informal social media channels, like ‘mommy’ blogs, Instagram accounts and online breastfeeding groups.”
Does AME have positive effects?
“There is some evidence that AME reduces infant formula supplementation in the first few days after birth and promotes more exclusive breastfeeding,” says Jill. “That’s good news, since longer, more exclusive breastfeeding has important health benefits for both parent and baby, and is good for the economy and environment.”
AME might reduce infant formula use because it allows women/birthing people to freeze expressed milk before their baby is born. This gives them an option other than infant formula or donor human milk (which is not always available) if their baby needs a small amount of extra milk after birth. This might be necessary if breastfeeding is not going well or parent and baby are separated due to medical complications.
AME can also increase an individual’s confidence and comfort with breastfeeding, leading to them feeling more prepared for their baby’s arrival. “AME seems to be a catalyst to get people thinking through the mechanics and logistics of breastfeeding,” says Jill.
Some women/birthing people have even reported that AME seemed to contribute to having more breast milk after they give birth, too.
What is Jill’s research looking at?
Until now, AME has mainly been studied in women/birthing people with diabetes. This group has a high risk of using infant formula right after birth, because the babies can have blood sugar regulation issues that require immediate feeding. In addition, those with diabetes may have hormonal issues caused by diabetes which negatively affect milk production.
However, Jill has decided to study AME among other groups at risk for sub-optimal breastfeeding outcomes. One of the groups she has focused on in her research are people whose BMI before pregnancy is 25 or higher (classified as overweight or obese). “Compared to those with pre-pregnancy BMIs less then 25, these birthing people have a higher likelihood of breastfeeding problems, too, like low milk supply and early, unintended infant formula use,” says Jill.
This might be for both biological and societal reasons. “Birthing people with obesity can have a hormonal profile that interferes with the development of glandular (milk-making) tissue in the breast and problems with milk production within the available glandular breast tissue,” says Jill. Women who have excess weight or obesity may also have larger breasts, which means that positioning their baby for breastfeeding may be challenging. Societal reasons such as weight stigma bias might also play a role, as women with higher BMIs might feel uncomfortable with body exposure through breastfeeding. They may even feel judged by health providers about their weight and, therefore, less inclined to seek breastfeeding help if they need it.
What does Jill’s study involve?
Jill is recruiting 280 pregnant people with a pre-pregnancy BMI of at least 25 to take part in a study to see if AME can improve breastfeeding outcomes. “All participants are first-time parents, have no prior breastfeeding experience, and have no major health or pregnancy complications at the time of recruitment,” says Jill.
Participants meet with a lactation consultant once a week during their 37th to 40th week of pregnancy. This takes place over a Zoom video session and lets participants practise AME and ask the consultant for advice on AME and breastfeeding in general. “We then encourage participants to practise AME on their own, once or twice a day, for 10 minutes at a time,” says Jill.
Each day of the study, Jill’s team sends out automated text messages that ask participants questions about their AME practice. “Some people have questions when starting the study, such as whether practising AME will ‘use up’ their colostrum,” says Jill. “The answer to this is no. Milk is made on a continuous basis and colostrum continues until a few days after the birth.”
How is Jill controlling this study?
Out of Jill’s 280 participants, half are randomly assigned to the AME group and half are assigned to an attention control group – called this because the participants receive the same amount of attention from the staff as the AME group. The control group spend their study sessions watching videos on infant care and topics unrelated to antenatal milk expression or breastfeeding. This should mean that any differences in outcomes between the groups are due to the different content and not because only one group had the opportunity to interact with staff and ask questions.
What results has Jill found so far?
“We aren’t far enough in the study to analyse breastfeeding outcomes, so we don’t know yet if participants assigned to AME had better rates of exclusive breastfeeding or breastfed longer postpartum,” says Jill.
Reference
https://doi.org/10.33424/FUTURUM380
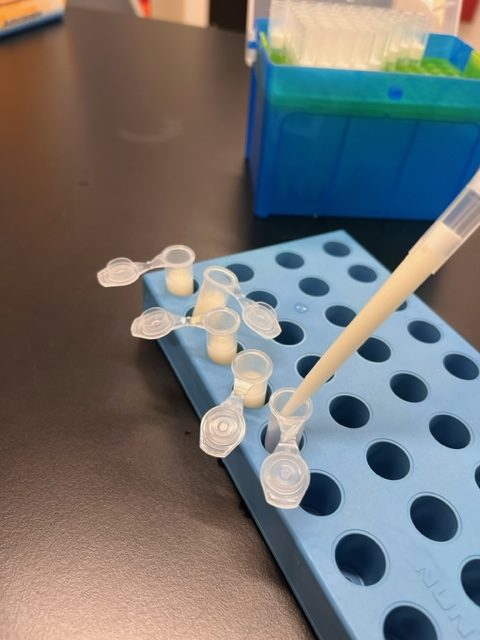
Examples of antenatal milk collected from 37-40 weeks of gestation from a second-time parent (who was not part of Jill’s AME study). Each container is 10 mL, and from a single day of expression. Note that the volume collected is significantly more than participants in Jill’s AME study typically express (~ <1-2 mL per expression session). Identifying information is blacked out on the containers, including bar code labels for milk transported to and temporarily stored at the birth hospital.
(Unless otherwise stated, all photos: © Jill Demirci)
However, Jill has had some feedback from participants already. She often hears that the study has increased people’s confidence to breastfeed, and that participants like having the time to get used to breastfeeding and ask questions before birth.
On the other hand, some are disappointed that they did not express as much milk as they expected to during the study. Jill and her team try to stress that everybody is different, and that AME is more about learning the hand expression skill than anything else. “Any milk expressed and banked is a bonus,” Jill adds.
What are the team’s next steps?
Many of the participants develop complications that lead to them giving birth earlier than the 37th week mark, meaning they do not even have a chance to start AME before they go into labour. “So, we’d like to explore the safety and efficacy of starting AME even earlier in pregnancy,” says Jill.
Jill’s team also collects breast milk samples from study participants, both before pregnancy and after birth. In the future, Jill would like to analyse these milk samples to look at changes in milk composition (nutrients and immune factors) over time.
Jill is also interested in pursuing more community-driven research in lactation. “This type of research is more likely to create actionable and sustainable solutions, rather than research that is conducted exclusively by academics,” says Jill. With more minds working together to improve breastfeeding outcomes, more women will hopefully be able to benefit from this research in the future.
 Dr Jill Demirci
Dr Jill Demirci
School of Nursing, University of Pittsburgh, USA
Field of research: Nursing Science
Research project: Investigating how antenatal milk expression affects breastfeeding outcomes among women with BMI 25 and over
Funders: National Institutes of Health (NIH), Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN), American Nurses Foundation (ANA)
About nursing science
Nursing scientists get to make a direct, positive impact on people’s lives, and they have the freedom to design their own career. Nursing scientists are trained nurses who have decided to branch into research. They create experiments, publish and write up their results in scientific papers, often teach, and aim to get their work translated into health policies, guidelines and public health campaigns.
What research opportunities will be open to the next generation of nursing scientists?
“Science is always evolving, and there are always new challenges!” says Jill. “There are so many big issues in healthcare to address, and nurse researchers can (and are) leading on so many of them. I think team science is going to be a model moving forward – currently most nurse researchers work individually and bring in outside co-investigators with given expertise on a particular project. In the future, we might see more interdisciplinary and community-based teams that bring complementary skills and work together over time on multiple projects. Another thing is big data (e.g., large national/ international and government-based datasets). I think nurses with expertise in this field will be in high demand, as this data can be powerful in guiding policy and action.”
Pathway from school to nursing science
• To become a nurse scientist, study science subjects such as biology, chemistry and anatomy while at school and at post- 16. “Many top nursing schools are looking for well-rounded high school students with some advanced placement courses, particularly in the sciences,” says Jill. You will need to complete a bachelor’s degree in nursing, before pursuing postgraduate study to become a researcher.
• “The nursing curriculum in universities is usually very prescribed, with core classes and clinical requirements,” says Jill. “However, I always think it’s a great idea to think about complementary interests and how taking additional courses outside the nursing curriculum might serve your nursing career.”
• If you can, try to study subjects outside of nursing to help you figure out where you want your nursing career to take you. At Jill’s university, undergraduate nursing students pursue certificates in subjects such as women’s studies, global health, philosophy, business and environmental sustainability.
• Jill recommends taking language courses if you are interested in travel and working in global health. “If you are interested in research then study biostatistics and take research-based courses,” she advises. “Humanity subjects – such as literature and history – can round out a science-heavy nursing curriculum and enrich your education immensely.”
Explore careers in nursing science
• Jill recommends looking at university summer programmes for high school students that allow you to work with faculty mentors to explore nursing skills and research. “You can also contact hospitals, community health organisations, or other areas where nurses work to see if shadowing opportunities are available,” says Jill.
• Many specialities in nursing have their own organisations and websites. “Reach out via email to an individual faculty member at a school of nursing or a nursing director at an organisation whose work resonates with you, and make that connection,” says Jill. “Sometimes, they have opportunities or may be willing to provide mentorship.”
• The American Nurses Association’s Nurse Focus has lots of useful information about what to think about when considering a career in nursing, as well as a checklist for selecting a nursing school.
Meet Jill
Who or what inspired you to pursue nursing?
Nursing appealed to me because it combined my love of science and my drive to make a positive impact through caring for people at vulnerable times in their lives. In nursing, there are so many opportunities for additional training, too. It is a career with almost endless possibilities, from the setting you work in, populations you work with, and the nature of your day-to-day work. You can chart your own course and change your direction if you choose.
What experiences have shaped your career?
While I was in nursing school, I had opportunities to work as a teaching assistant and an undergraduate researcher. My mentors really encouraged me to consider research and graduate school. They inspired and guided me in pursuing my PhD and a career in research.
I also had an undergraduate lecture on human lactation that fascinated me! Breastfeeding is not only about nutrition but connection, immunity, maternal health and well-being, infant behaviour, and so much more. When I became an obstetric nurse, I just assumed everyone would breastfeed for as long as possible because of all those amazing benefits. Then I saw how difficult breastfeeding could be, particularly without good support. Those experiences shaped my interests.
When I had my own children, I became intimately familiar with lactation challenges and how those challenges come to affect maternal psyche and permeate every aspect of life. I came back to the research field after their births with so many questions, plus an urgency and determination to pursue them. One of my research questions was around antenatal milk expression, which I had tried with great success with my first child.
What do you find rewarding about research in your field?
While clinical nursing, particularly in the hospital setting, can be very rewarding, it is also very demanding physically and emotionally. Sometimes there is limited room for individual creativity or change-making. Research, on the other hand, is a great fit for my personality. I love learning, reading and having the freedom to explore unanswered questions. I love that I design my own days and can work on several projects that are important to me at once. There is a lot of independent work in reading and writing, but it is interspersed with meetings and group work and chats. To me, a career in nursing research is the best of all worlds. Right now, I spend a good portion of my time writing grants, meeting with research staff, collaborating with other researchers, writing research papers, and presenting at health conferences. I also spend time doing clinical lactation consulting, mentoring PhD students, teaching undergraduate and graduate courses, and working on clinical innovations in the lactation field. It is so rewarding, and every day is different!
What are your proudest career achievements so far?
My proudest moments are hearing from participants in our studies that our interventions made a difference in their breastfeeding relationships and experience as a mother/parent. It has also been rewarding to publish our findings and see our data spur new investigations and be cited in clinical breastfeeding recommendations.
I’d say that even more so than any achievements, it’s the process that I’m proud of. I love working with and mentoring undergraduate and graduate students in research. It’s so gratifying to realise that they will go on to collectively influence healthcare in a bigger way than I could ever do as a single individual.
Jill’s top tips
1. Worry less about a perfect GPA/exam score and focus on learning. Take courses and pursue enrichment opportunities outside of what you are typically inclined. You might surprise yourself!
2. You can chart your own course – your career is uniquely yours and it doesn’t have to look like anyone else’s. Play to your strengths and don’t be afraid to dive deeply into what excites you.
3. We spend a good portion of our lives working – make sure it is on something you love.
Do you have a question for Jill?
Write it in the comments box below and Jill will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)