How research fields are joining forces to protect healthcare systems
Healthcare-associated infections and antimicrobial resistance are two of the greatest threats to global healthcare systems. Dealing with them cannot rely upon medicine alone. Instead, social, technological and computational innovations need to be integrated. An interdisciplinary team of researchers from Imperial College London, UK, and the UK Health Security Agency is rising to this challenge
GLOSSARY
MICROBE – a single-celled organism
PATHOGEN – a microbe that causes disease, such as some bacteria
ANTIMICROBIAL – an agent that destroys or inhibits microbes, including bacteria, fungi and viruses
ANTIBIOTIC – an agent used to combat bacteria
ARTIFICIAL INTELLIGENCE – computer systems that can ‘learn’ to perform tasks
BIOSENSOR – a device that senses or measures a particular biological trait
EPIDEMIOLOGY – the study of diseases
PROTEOMICS – the large-scale study of proteins
Although hospitals and healthcare facilities are the best tools we have for combating illness, they can also be hotbeds for infectious diseases, including drug resistant ones. To address the problem, a diverse team of scientists has been assembled to investigate this issue from fields such as medicine, biology, social sciences and technology.
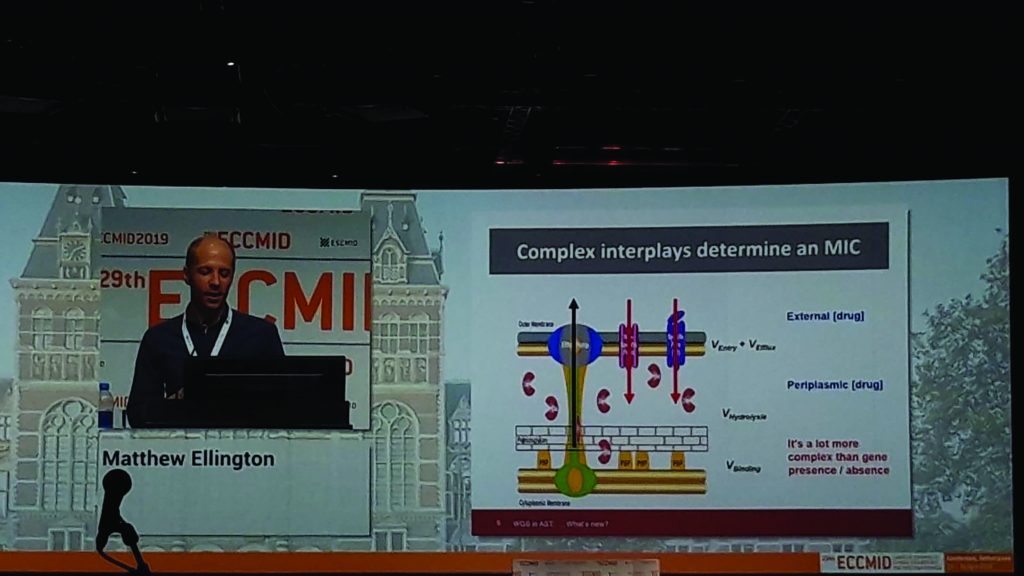
Professor Alison Holmes at Imperial College London and Dr Matt Ellington at the UK Health Security Agency (formerly Public Health England) lead a Health Protection Research Unit (HPRU) focused on two of the greatest threats to healthcare systems around the world – healthcare-associated infections and antimicrobial resistance. The HPRU brings together academic researchers and clinical practitioners to build a more effective healthcare system.
HCAIS AND AMR
Healthcare-associated infections (HCAIs) occur when a patient in the health system for one treatment then becomes infected by another disease. “Interactions with healthcare should make people better, not worse, so HCAIs are a real problem,” says Alison.
Antimicrobial resistance (AMR) occurs when pathogens evolve to no longer be affected by a particular antimicrobial drug, making disease harder to treat. “So much of modern medicine depends on working antimicrobials,” Alison explains. “If antibiotics cease to work, medicine could go back to the Dark Ages.”
AMR is not an emerging issue; it is already a global problem, referred to as the ‘silent pandemic’ as the public rarely hears about it. If one pathogen becomes resistant to one antibiotic in one country, the resistant strain will soon spread around the globe. And many pathogens have evolved to become resistant to multiple drugs. “We now see resistance in a wide range of bacteria, against a wide range of antibiotics, throughout the world,” says Alison.
ANTIMICROBIAL STEWARDSHIP
Alison advocates for the concept of ‘antimicrobial stewardship’, which means only using antimicrobial drugs when they are necessary. “Antimicrobial resistance is natural, and we can’t stop it,” she says, “but we can slow it down.” We should all take responsibility for antimicrobial stewardship. Only use antibiotics if they are essential and follow the advice of healthcare professionals. Practice good hygiene, as regular handwashing will stop transmission. And have vaccinations to reduce your chances of getting infections in the first place.
THE HPRU
“Research into AMR has to be collaborative to be successful,” says Alison. This is why the HPRU is an interdisciplinary partnership between Imperial College London and the UK Health Security Agency. “This partnership means that our research is grounded in public health priorities, not just academic interest,” she explains. “We provide an evidence base which has already influenced government guidelines on controlling infections.”
Using expertise from a variety of fields, the HPRU is addressing HCAIs and AMR via four complementary research themes: 1) Priority pathogens, 2) Precision prescribing, 3) Practice, design and engineering, and 4) Population health and policy.
PRIORITY PATHOGENS
To assess the risks of AMR, it is important to know how different microbe species behave and adapt. Dr Elita Jauneikaite works on identifying priority pathogens – those most likely to develop antimicrobial resistance and cause issues for public health. Many of these pathogens can cause severe infections and are especially dangerous to people with compromised immune systems.
Elita’s team is very diverse, to ensure the project is approached from multiple angles. “We have experts in bacterial pathogenesis, proteomics and molecular biology, alongside clinicians, epidemiologists, mathematical modellers and data analysts,” she says. “This diversity gives us a much better overall picture of how different aspects of priority pathogens interact and influence each other.”
This variety in research expertise results in a wide range of scientific techniques being used, to understand how bacterial populations change over time and how this affects patients. Bioinformatics (a field which involves the processing of large quantities of biological data) methods are used to detect antimicrobial resistance genes and how they mutate over time. Molecular biology techniques can test these mutations in the lab to see which are the most effective at resisting antimicrobials. “As well as lab studies, we also analyse anonymised patient data to better understand if particular patient populations are especially at risk to specific bacteria strains,” says Elita.
Elita hopes that her team’s method of combining patient data with biological research into specific pathogens can set a framework for further investigation into how antimicrobial resistance is transmitted between pathogens and between patients.
PRACTICE, DESIGN AND ENGINEERING
Though an understanding of the biological science behind HCAIs and AMR is fundamental, it doesn’t capture every aspect of transmission. Dr Esmita Charani is focusing on the social and physical environment of the healthcare network and assessing how it could be improved to lower risks of infection and transmission.
The behaviours of healthcare professionals, patients and the public depend upon attitudes towards infection and antibiotic use. “Ever since their discovery in World War II, antibiotics have been heralded as ‘miracle drugs’,” says Esmita. This has resulted in their wide-spread use as the simplest way to cure most illnesses.
Before attempting to change these behaviours, Esmita and her team are hoping to understand the motivations behind them. “We have to create the right environment to support individuals to make the right decisions,” she says. This can involve simple measures such as promoting hand washing in hospitals, as well as more complex measures such as the development of bespoke prescription charts or apps to help doctors prescribe antibiotics appropriately. “We also need to communicate the risks of AMR to the public, including the importance of using antibiotics only when necessary and when prescribed,” says Esmita.
The physical environment of hospitals is also important. Esmita advocates the use of ‘smart engineering’ to reduce infection risk, such as improving ventilation, reducing ‘touch surfaces’ (e.g. door handles and taps) and constructing clinical surfaces from materials that do not harbour microbes.
PRECISION PRESCRIBING
More advanced healthcare techniques rely on sophisticated data collection. Dr Tim Rawson is exploring how technologies such as artificial intelligence and biosensors can help combat HCAIs and AMR. “A huge amount of data is generated for every patient within a healthcare system,” says Tim. “However, much of this data will not be integrated into larger datasets, due to difficulties in processing and interpreting it.”
Tim believes that addressing this could help doctors prescribe antimicrobials more appropriately and precisely. “Antimicrobial prescribing is complex,” he explains. “By using data that incorporates this complexity for individual patients, prescribers will be able to make more accurate decisions about which antibiotic to use and how long it should be used for.” These data-supported decisions would be better for the individual patient and would also reduce the risk of AMR.
The sophistication of these decisions can be taken a step further with artificial intelligence. “An algorithm could analyse hundreds of variables and summarise them into a single probability score for ‘risk of bacterial infection’, which allows the prescriber to decide on the appropriateness of antibiotic prescription,” says Tim.
Technology can also encourage optimal antibiotic prescription through the use of biosensors, which measure the concentration of microbes and antimicrobials in a patient’s blood. This allows doctors to track how the antibiotic is faring within the body after administering it and rapidly adjust the dosage to ensure optimal efficiency. Tim believes that integrating these technologies into standard healthcare routines could lead to a much more precise approach to treating microbial infections.
POPULATION HEALTH AND POLICY
Dr Nina Zhu is working on maximising the usefulness of data collected within healthcare systems, through data linkage, systems modelling and dynamics, and network analysis. “Rather than tracking diseases, we are tracking patients, by linking data generated from different sources,” she says. “This involves assessing policy environments and mapping patient movement and networks, to inform the design of health interventions.”
Nina works with ‘whole systems integrated care’, which links multiple health sectors across north-west London. “This integration has helped us study how infections emerge in the community, how they are managed, and whether treatment succeeds or fails,” says Nina. “It also provides evidence for whether infections are associated with movement of patients within or between hospitals.”
This system came into its own during the COVID-19 pandemic. “The first challenge was to ascertain which COVID cases were HCAIs,” says Nina. “We developed a system to automatically flag any patients whose virology test results confirmed they had caught the virus within hospital and modelled their movements within the hospital to identify which wards saw the most transmission events.”
The team also reviewed existing literature of previous pandemics and developed a holistic instrument to guide future pandemic response, incorporating social, political and technological considerations.
Reference
https://doi.org/10.33424/FUTURUM200
MICROBE – a single-celled organism
PATHOGEN – a microbe that causes disease, such as some bacteria
ANTIMICROBIAL – an agent that destroys or inhibits microbes, including bacteria, fungi and viruses
ANTIBIOTIC – an agent used to combat bacteria
ARTIFICIAL INTELLIGENCE – computer systems that can ‘learn’ to perform tasks
BIOSENSOR – a device that senses or measures a particular biological trait
EPIDEMIOLOGY – the study of diseases
PROTEOMICS – the large-scale study of proteins
Although hospitals and healthcare facilities are the best tools we have for combating illness, they can also be hotbeds for infectious diseases, including drug resistant ones. To address the problem, a diverse team of scientists has been assembled to investigate this issue from fields such as medicine, biology, social sciences and technology.
Professor Alison Holmes at Imperial College London and Dr Matt Ellington at the UK Health Security Agency (formerly Public Health England) lead a Health Protection Research Unit (HPRU) focused on two of the greatest threats to healthcare systems around the world – healthcare-associated infections and antimicrobial resistance. The HPRU brings together academic researchers and clinical practitioners to build a more effective healthcare system.
HCAIS AND AMR
Healthcare-associated infections (HCAIs) occur when a patient in the health system for one treatment then becomes infected by another disease. “Interactions with healthcare should make people better, not worse, so HCAIs are a real problem,” says Alison.
Antimicrobial resistance (AMR) occurs when pathogens evolve to no longer be affected by a particular antimicrobial drug, making disease harder to treat. “So much of modern medicine depends on working antimicrobials,” Alison explains. “If antibiotics cease to work, medicine could go back to the Dark Ages.”
AMR is not an emerging issue; it is already a global problem, referred to as the ‘silent pandemic’ as the public rarely hears about it. If one pathogen becomes resistant to one antibiotic in one country, the resistant strain will soon spread around the globe. And many pathogens have evolved to become resistant to multiple drugs. “We now see resistance in a wide range of bacteria, against a wide range of antibiotics, throughout the world,” says Alison.
ANTIMICROBIAL STEWARDSHIP
Alison advocates for the concept of ‘antimicrobial stewardship’, which means only using antimicrobial drugs when they are necessary. “Antimicrobial resistance is natural, and we can’t stop it,” she says, “but we can slow it down.” We should all take responsibility for antimicrobial stewardship. Only use antibiotics if they are essential and follow the advice of healthcare professionals. Practice good hygiene, as regular handwashing will stop transmission. And have vaccinations to reduce your chances of getting infections in the first place.
THE HPRU
“Research into AMR has to be collaborative to be successful,” says Alison. This is why the HPRU is an interdisciplinary partnership between Imperial College London and the UK Health Security Agency. “This partnership means that our research is grounded in public health priorities, not just academic interest,” she explains. “We provide an evidence base which has already influenced government guidelines on controlling infections.”
Using expertise from a variety of fields, the HPRU is addressing HCAIs and AMR via four complementary research themes: 1) Priority pathogens, 2) Precision prescribing, 3) Practice, design and engineering, and 4) Population health and policy.
PRIORITY PATHOGENS
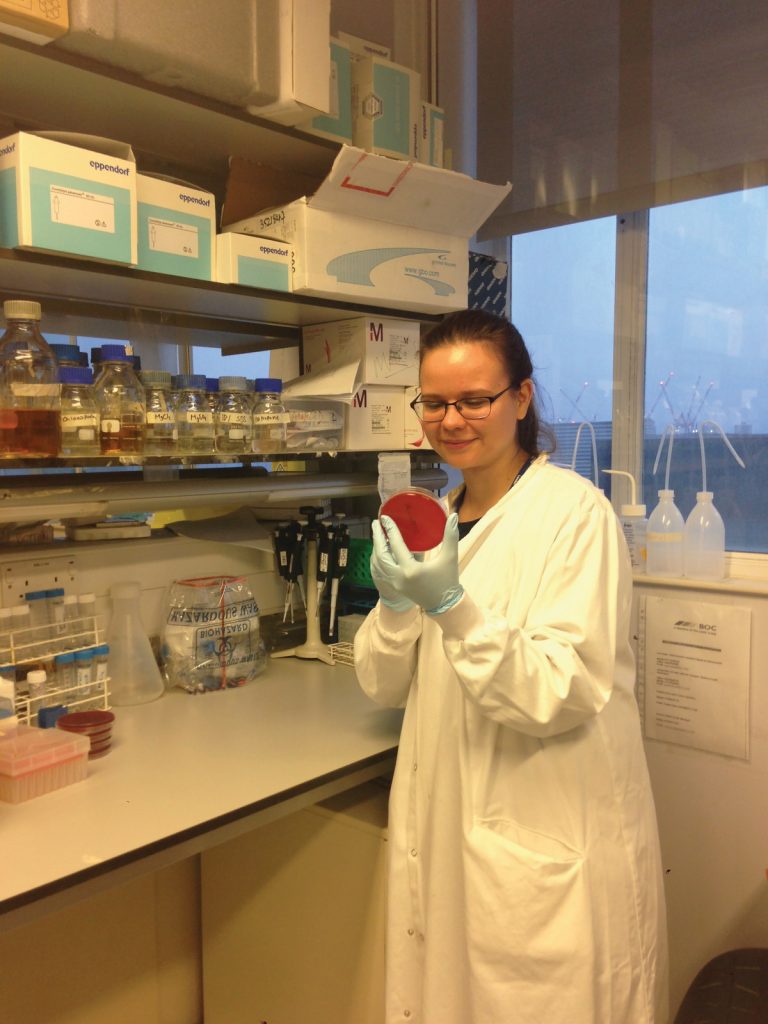
To assess the risks of AMR, it is important to know how different microbe species behave and adapt. Dr Elita Jauneikaite works on identifying priority pathogens – those most likely to develop antimicrobial resistance and cause issues for public health. Many of these pathogens can cause severe infections and are especially dangerous to people with compromised immune systems.
Elita’s team is very diverse, to ensure the project is approached from multiple angles. “We have experts in bacterial pathogenesis, proteomics and molecular biology, alongside clinicians, epidemiologists, mathematical modellers and data analysts,” she says. “This diversity gives us a much better overall picture of how different aspects of priority pathogens interact and influence each other.”
This variety in research expertise results in a wide range of scientific techniques being used, to understand how bacterial populations change over time and how this affects patients. Bioinformatics (a field which involves the processing of large quantities of biological data) methods are used to detect antimicrobial resistance genes and how they mutate over time. Molecular biology techniques can test these mutations in the lab to see which are the most effective at resisting antimicrobials. “As well as lab studies, we also analyse anonymised patient data to better understand if particular patient populations are especially at risk to specific bacteria strains,” says Elita.
Elita hopes that her team’s method of combining patient data with biological research into specific pathogens can set a framework for further investigation into how antimicrobial resistance is transmitted between pathogens and between patients.
PRACTICE, DESIGN AND ENGINEERING
Though an understanding of the biological science behind HCAIs and AMR is fundamental, it doesn’t capture every aspect of transmission. Dr Esmita Charani is focusing on the social and physical environment of the healthcare network and assessing how it could be improved to lower risks of infection and transmission.
The behaviours of healthcare professionals, patients and the public depend upon attitudes towards infection and antibiotic use. “Ever since their discovery in World War II, antibiotics have been heralded as ‘miracle drugs’,” says Esmita. This has resulted in their wide-spread use as the simplest way to cure most illnesses.
Before attempting to change these behaviours, Esmita and her team are hoping to understand the motivations behind them. “We have to create the right environment to support individuals to make the right decisions,” she says. This can involve simple measures such as promoting hand washing in hospitals, as well as more complex measures such as the development of bespoke prescription charts or apps to help doctors prescribe antibiotics appropriately. “We also need to communicate the risks of AMR to the public, including the importance of using antibiotics only when necessary and when prescribed,” says Esmita.
The physical environment of hospitals is also important. Esmita advocates the use of ‘smart engineering’ to reduce infection risk, such as improving ventilation, reducing ‘touch surfaces’ (e.g. door handles and taps) and constructing clinical surfaces from materials that do not harbour microbes.
PRECISION PRESCRIBING
More advanced healthcare techniques rely on sophisticated data collection. Dr Tim Rawson is exploring how technologies such as artificial intelligence and biosensors can help combat HCAIs and AMR. “A huge amount of data is generated for every patient within a healthcare system,” says Tim. “However, much of this data will not be integrated into larger datasets, due to difficulties in processing and interpreting it.”
Tim believes that addressing this could help doctors prescribe antimicrobials more appropriately and precisely. “Antimicrobial prescribing is complex,” he explains. “By using data that incorporates this complexity for individual patients, prescribers will be able to make more accurate decisions about which antibiotic to use and how long it should be used for.” These data-supported decisions would be better for the individual patient and would also reduce the risk of AMR.
The sophistication of these decisions can be taken a step further with artificial intelligence. “An algorithm could analyse hundreds of variables and summarise them into a single probability score for ‘risk of bacterial infection’, which allows the prescriber to decide on the appropriateness of antibiotic prescription,” says Tim.
Technology can also encourage optimal antibiotic prescription through the use of biosensors, which measure the concentration of microbes and antimicrobials in a patient’s blood. This allows doctors to track how the antibiotic is faring within the body after administering it and rapidly adjust the dosage to ensure optimal efficiency. Tim believes that integrating these technologies into standard healthcare routines could lead to a much more precise approach to treating microbial infections.
POPULATION HEALTH AND POLICY
Dr Nina Zhu is working on maximising the usefulness of data collected within healthcare systems, through data linkage, systems modelling and dynamics, and network analysis. “Rather than tracking diseases, we are tracking patients, by linking data generated from different sources,” she says. “This involves assessing policy environments and mapping patient movement and networks, to inform the design of health interventions.”
Nina works with ‘whole systems integrated care’, which links multiple health sectors across north-west London. “This integration has helped us study how infections emerge in the community, how they are managed, and whether treatment succeeds or fails,” says Nina. “It also provides evidence for whether infections are associated with movement of patients within or between hospitals.”
This system came into its own during the COVID-19 pandemic. “The first challenge was to ascertain which COVID cases were HCAIs,” says Nina. “We developed a system to automatically flag any patients whose virology test results confirmed they had caught the virus within hospital and modelled their movements within the hospital to identify which wards saw the most transmission events.”
The team also reviewed existing literature of previous pandemics and developed a holistic instrument to guide future pandemic response, incorporating social, political and technological considerations.
THE NIHR HEALTH PROTECTION RESEARCH UNIT IN HEALTHCARE-ASSOCIATED INFECTIONS AND ANTIMICROBIAL RESISTANCE
INSTITUTIONS: Imperial College London and the UK Health Security Agency (formerly Public Health England), UK
FIELD OF RESEARCH: Healthcare-Associated Infections, Antimicrobial Resistance
FUNDER: National Institute for Health Research
INSTITUTIONS: Imperial College London and the UK Health Security Agency (formerly Public Health England), UK
FIELD OF RESEARCH: Healthcare-Associated Infections, Antimicrobial Resistance
FUNDER: National Institute for Health Research
EXPLORE A CAREER IN ANTIMICROBIAL RESISTANCE RESEARCH
AMR is a serious threat to global healthcare systems that needs to be tackled from a diverse range of perspectives. You could address the issue clinically, working as a doctor or pharmacist. You could study the biological processes of AMR as a microbiologist or epidemiologist. You could develop new technologies to monitor AMR as a bioengineer or analyse the results of AMR studies as a data scientist. You could investigate our relationship with antimicrobial drugs from a social science point of view as an anthropologist or economist. Or you could work in public health to influence government policy.
The HPRU recognises the importance of encouraging people from all walks of life to get involved in AMR research. They welcome people to get in touch and find out more: www.imperial.ac.uk/medicine/hpru-amr
• As highlighted by the researchers in the HPRU, there are many different pathways into AMR research.
• At school, STEM subjects will be valuable for following any route into AMR research. Most scientific research requires computer coding skills for analysing data, so the team advise learning to code. Biology and/or chemistry will be essential for many university courses that could lead to AMR research. Maths will be beneficial if you will be dealing with data. English or foreign languages will provide useful communication skills, but these are not typically requirements for STEM university courses.
• At university, courses such as medicine, molecular biology, epidemiology, pharmacology, bioengineering, mathematics and anthropology could all lead to a career in AMR research.
• Alison highlights that effective communication is needed to change public attitudes to antimicrobials. Subjects such as public health, journalism and politics are therefore all relevant to addressing the increasing global threat of AMR.
MEET THE TEAM

PROFESSOR ALISON HOLMES
PROFESSOR OF INFECTIOUS DISEASES, IMPERIAL COLLEGE LONDON
DIRECTOR OF THE HPRU
I have always found infectious diseases the most interesting area of medicine. It links diseases to the environment, and as a doctor of infectious diseases you have to be interested in transmission, vectors and epidemiology as well as the disease itself. I find this whole-system approach produces some of the best doctors.
Being the Director of the HPRU is just one of my roles, all of which involve talking to a wide range of people, from international leaders to NHS colleagues on the wards, to researchers at every stage of their academic career. Sharing ideas with these people is one of the joys of my work.
Every day of work is varied. I always have meetings with my research team and other colleagues to attend. I also spend a lot of time reading – draft manuscripts summarising our work, grant applications for new funding, PhD theses that I am examining… There are a lot of demands on my time, so the support of my core team has been really important.
I love being surrounded by incredibly talented colleagues and seeing them grow and flourish. It is fantastic to collaborate with so many brilliant experts in different fields, and including behavioural research and bioengineering research into our group has been wonderful.
Initially, it was very challenging to raise the profile of AMR and the need to address how we use antibiotics. It was apparent to me that we needed greater focus and leadership, and much more research into the issue. Finally, it is becoming a national and global research priority.
I lived in many different places growing up. In every environment, my father shared his interest in natural history and his extraordinary knowledge and sharp observation skills, which inspired me to become a scientist.
Enthusiasm, genuine interest and persistence have made me a successful scientist. I have made the most of opportunities and have learnt from those around me. I have also helped support others through collaborations and advancing their interests and careers.

DR MATT ELLINGTON
UK HEALTH SECURITY AGENCY LEAD FOR THE HPRU
At school I enjoyed biology and biochemistry, so I chose a degree with flexible core modules in life sciences. At university, my imagination was caught by a lecture on microbial bioenergetics. I completed a summer placement project with the lecturer, Professor David Richardson, and subsequently a final-year practical project in his lab. As well as building my technical skills, David inspired my inquisitiveness through discussing ideas and theories and finding ways to test them.
I then completed a PhD in microbial bioenergetics and molecular biology, after which I was recruited to investigate antimicrobial resistant bacteria. This role opened my eyes to the scale and breadth of research activity taking place around AMR.
I became qualified as a clinical scientist and developed my bioinformatics and computer coding skills so I could analyse whole genome sequence data. As my work became more managerial, it cemented my belief in the importance of having a wider public health science workforce partnering closely with the UK Health Security Agency.
In the national AMR reference laboratory we receive samples of bacteria from hospitalised patients and test them for unusual antimicrobial resistances, while conducting research into how to detect new forms of resistance. We also investigate infectious outbreaks and analyse how bacteria spread between individuals, and we examine new antimicrobial drugs to determine how microbes may develop resistance to them.
I think that interpreting our results is the most interesting part of my research, trying to determine ‘what does it mean?’ My work involves lots of meetings with colleagues to analyse data, discuss our results or plan our next steps. There are also always technical problems to solve when conducting research.
I think my interest in the ‘technical details’ and my desire to understand things have helped my success. I have always wanted to do something helpful for society and future generations.
As a pre-teen I was very into building things from LEGO and Meccano and building remote-controlled cars. As a teenager I loved music, as well as football, cycling and other outdoor pursuits.

DR ELITA JAUNEIKAITE
MICROBIOLOGIST
PRIORITY PATHOGENS RESEARCH LEAD
My undergraduate degree was in microbiology, with a year of professional training in industry. I then gained further laboratory research experience in molecular epidemiology at Public Health England. This helped me to see how useful such research can be, which encouraged me to pursue a PhD.
My previous studies and research prepared me for my current role leading the Priority Pathogens team. They provided opportunities to learn new techniques, work with researchers from different backgrounds, manage multiple multi-disciplinarity projects and pursue my research interests.
Being a research scientist involves many roles, which often all come at once. Though this can be challenging, it is also what makes scientific research so engaging. As a senior researcher, I manage other researchers and students as well as collaborating with clinicians who work on the front lines of microbial outbreaks in hospitals.
A typical day for a researcher is a busy one! I specialise in bacterial genomic analysis, so when I’m not talking to colleagues or writing up research, I’m linking to the university’s supercomputer to analyse data for new discoveries.
A scientist must be curious and driven to ask ‘why?’ The ability to absorb and process large amounts of information and to find patterns and answers, and the tenacity to not give up are also useful. And they must be able to work with other researchers.
I loved reading books as a child, especially books about nature. I loved observing and learning things, organising events and going on nature walks. I think it was my love of solving puzzles and interest in the natural world that led me to become a scientist.
Outside of work, I enjoy spending time with my family, travelling and meeting new people. I still retain my love for nature and animals.

DR ESMITA CHARANI
CLINICAL PHARMACIST
PRACTICE, DESIGN AND ENGINEERING RESEARCH LEAD
I meandered my way into research and science. I always wanted to be a journalist or author but became inspired by the people interested in sharing the knowledge and skills they have gained through research.
I studied pharmacy and then completed an MSc in Infectious Diseases. After a few years working in antimicrobial stewardship and medicines information, I applied for a research job even though I had no research experience. Over the last ten years I have developed my research career and completed a PhD, which focused on applying social science research to understand how and why people use antibiotics, and implications for their long-term effectiveness.
I love my research role as there is never a dull day. I get to feed my curiosity and follow ideas and questions that interest me. I have developed fantastic collaborations with colleagues around the world from different professions – when it comes to infectious diseases, itis important to work across geographic and cultural boundaries. It is extremely rewarding to contribute to positive outcomes in healthcare.
Early in the pandemic I volunteered in our vaccination clinics for staff, which was very rewarding. I also supported the research teams in the hospital conducting studies about diagnosis and management of COVID-19.
Curiosity, patience and tenacity are important skills for a scientist. It is also vital to build strong relationships with colleagues, to work together and learn from each other.
As a child, I loved reading. My family also travelled a lot, which was great as I enjoy being on the road in search of adventure, but meant I frequently had to change schools. I even missed out on school for a year!
As well as travelling, I enjoy cooking and baking for my friends and family. When I was on-call as a pharmacist, I taught myself to make jewellery to keep me awake on night shifts. I have made lots of pieces from silver and semi-precious stones for myself, relatives and friends.

DR TIM RAWSON
CLINICAL DOCTOR IN INFECTIOUS DISEASES AND MEDICAL MICROBIOLOGY
PRECISION PRESCRIBING RESEARCH LEAD
I have wanted to pursue a career in infectious diseases since my first year of medical school. During my undergraduate training I found that I enjoyed academic writing and research, which cemented my desire to explore ways of linking clinical practice with academia. As part of my PhD, I explored the role of artificial intelligence and biosensor technologies in delivering precision antimicrobial therapy.
I am currently completing clinical training alongside academic research. It can be challenging to balance my time between increasing clinical and academic commitments as I progress in my career, but fortunately the HPRU supports me in this.
Research-focused days can be incredibly varied. We work on a broad range of subjects, from clinical trials of medical devices to the development of new technologies. Leading the Precision Prescribing team, a lot of my time is dedicated to developing research ideas and supporting members of the team.
I love identifying clinically important challenges and addressing them through academic research. It’s satisfying to see a study develop from an initial idea to meaningful results. I also feel very fortunate to work with such a friendly group of people, which fosters a culture of collaboration.
I am lucky in that I really enjoy what I do. Scientists need enthusiasm to learn new skills and think differently about things. They also need to have fairly thick skin, as you will inevitably face criticism of your work and the methods you chose, but it is important to learn from this feedback.
I was always interested in science and making things when I was growing up. My father is a joiner and I worked as a labourer during my summer holidays. Although I’m not very good at carpentry, I enjoyed the practical aspect of making things and this has translated to some of the technology development work I have been involved in over the years.
Outside of work, I aim to enjoy the outdoors as much as possible. I play golf (socially, not competitively) and scuba dive. In recent years I have been learning to rock climb, travelling around the UK to Portland and the Peak District to test my skills.

DR NINA ZHU
EPIDEMIOLOGIST
POPULATION HEALTH AND POLICY RESEARCH LEAD
My background is in biomedical engineering, which set the foundation for me to become a quantitative researcher. Prior to joining the HPRU, I explored different fields of public health, and completed a PhD that combined systems theory with research into infectious disease. I was attracted to the HPRU’s multidisciplinary team and the fact that it is a fast track to real-life health data.
A typical day involves number crunching as I analyse data and a lot of meetings with clinicians and researchers. I work with scientists from various fields – doctors, pharmacists, microbiologists…
I enjoy the process of answering questions using real-life data – I like solving puzzles. The challenge lies in ensuring that I interpret my findings appropriately as it is important to understand the limitations and the wider context of the data.
Curiosity drove me to become a scientist. I loved detective novels when I was younger, and have always been intrigued by unanswered questions. I am always determined to find out ‘why’. I still enjoy reading in my spare time, as well as going to the gym.
THE TEAM’S TOP TIPS
01 Find what feeds your curiosity and passion – do what inspires and fascinates you. You should enjoy what you do!
02 Try hard, be flexible and work with great people.
03 Don’t try to walk in the shoes of others. Do what is right for you. If something interests you, pursue it. But if you lose the interest, shift your focus elsewhere and don’t punish yourself for making mistakes.
Do you have a question for Alison, Matt, Elita, Esmita, Tim or Nina?
Write it in the comments box below and Alison, Matt, Elita, Esmita, Tim or Nina will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)