Lighting up cancer: innovation in paediatric surgery
Surgically removing cancer tumours can be a risky procedure – bodily tissues that the cancer grows on can be damaged in the process, and leaving any part of the tumour behind can lead to the cancer coming back. Dr Stefano Giuliani and his team at the University College London (UCL) Great Ormond Street Institute of Child Health in the UK are developing a ground-breaking technique that literally ‘lights up’ the cancer cells, making removal much easier.
TALK LIKE A NEONATAL AND PAEDIATRIC SURGEON
Antibody — protein molecules found in the blood that aid the recognition of pathogens and other harmful substances
Biomedicine — the branch of medicine that involves applying biological and biochemical research to medical research and practice
Cancer — a disease in which certain cells in the body grow uncontrollably and spread to other parts of the body
Fluorescence — the emission of light by a substance that has absorbed light or other electromagnetic radiation
In vitro — a process that takes place outside of a living organism (e.g., in a tissue culture dish)
Neonatal — relating to newborn children
Neuroblastoma — a type of cancer that forms from certain immature nerve cells
Paediatric — the branch of medicine relating to children and the diseases that affect them
Tissue — any of the materials that make up the body (e.g., specialised cells and their products)
Tumour — a mass of tissue formed when cells grow uncontrollably and which can be benign or malignant
Cancers come in a wide array of shapes and sizes and can affect different parts of the body in different ways. High-risk neuroblastoma is a type of cancer that occurs principally in babies and young children. It affects around 100 children every year in the UK and in its more aggressive form has a low survival rate. Neuroblastoma occurs when specialised nerve cells, called neuroblasts, are left behind from the child’s time in the womb and become cancerous. “High-risk neuroblastoma is an aggressive cancer, which has often spread to multiple organs by the time of diagnosis,” says Dr Stefano Giuliani. Stefano is a surgeon at UCL Great Ormond Street Institute of Child Health (ICH) in London. He is working on a pioneering research study that could dramatically improve survival rates for children with this cancer.
Challenges of surgery
Treatment for neuroblastoma involves surgically removing the entire tumour, but this is a challenging task even for the most experienced surgeons. “The neuroblastoma grows around the largest and most critical vessels, nerves and organs in the body,” explains Stefano. “This raises the risk of damaging these tissues during surgery, which can lead to dangerous situations such as severe bleeding.”
Currently, it is not easy to tell the difference between cancerous tissue and normal healthy tissues during surgery, which is why this procedure is so challenging. “There is a need to develop a tumour-specific detection strategy to help surgeons easily see tumour cells versus normal anatomical structures,” says Stefano. This need forms the foundation of his research project.
Fluorescence-guided surgery
Fluorescence-guided surgery (FGS) could provide the solution to solving this issue. “FGS is possibly one of the greatest innovations in surgery,” says Stefano. “We are developing specific fluorescence probes which can clearly highlight cancer cells.” Fluorescent molecules are those that ‘light up’, emitting a certain wavelength of light when exposed to either visible light or other wavelengths such as ultraviolet or infrared.
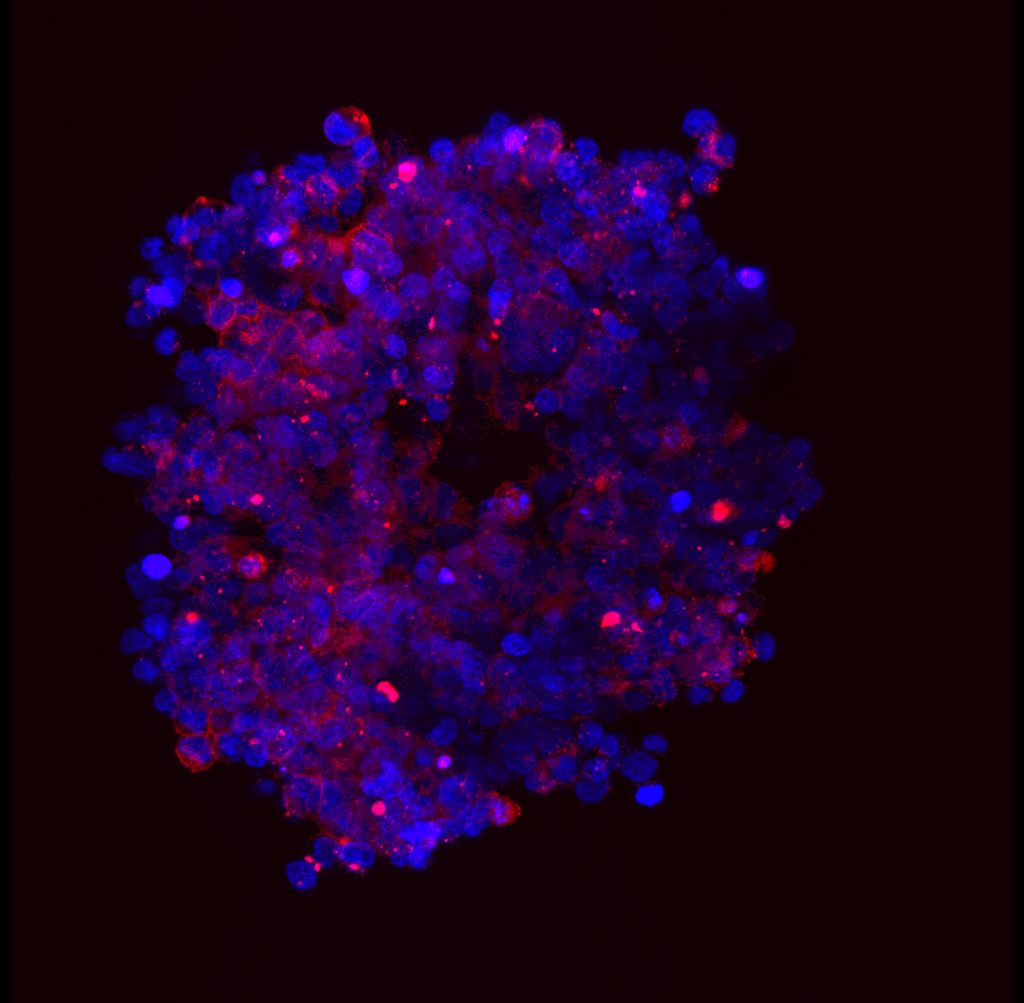
These fluorescence probes are formed using a clever biochemical technique. The main way the body’s immune system naturally detects pathogens or cancers is via the use of antibodies – molecules whose shape matches other molecules only found on the surface of specific harmful cells. Biomedical scientists have found the antibody specific to neuroblastoma and can modify this in the lab to attach a fluorescent particle to it.
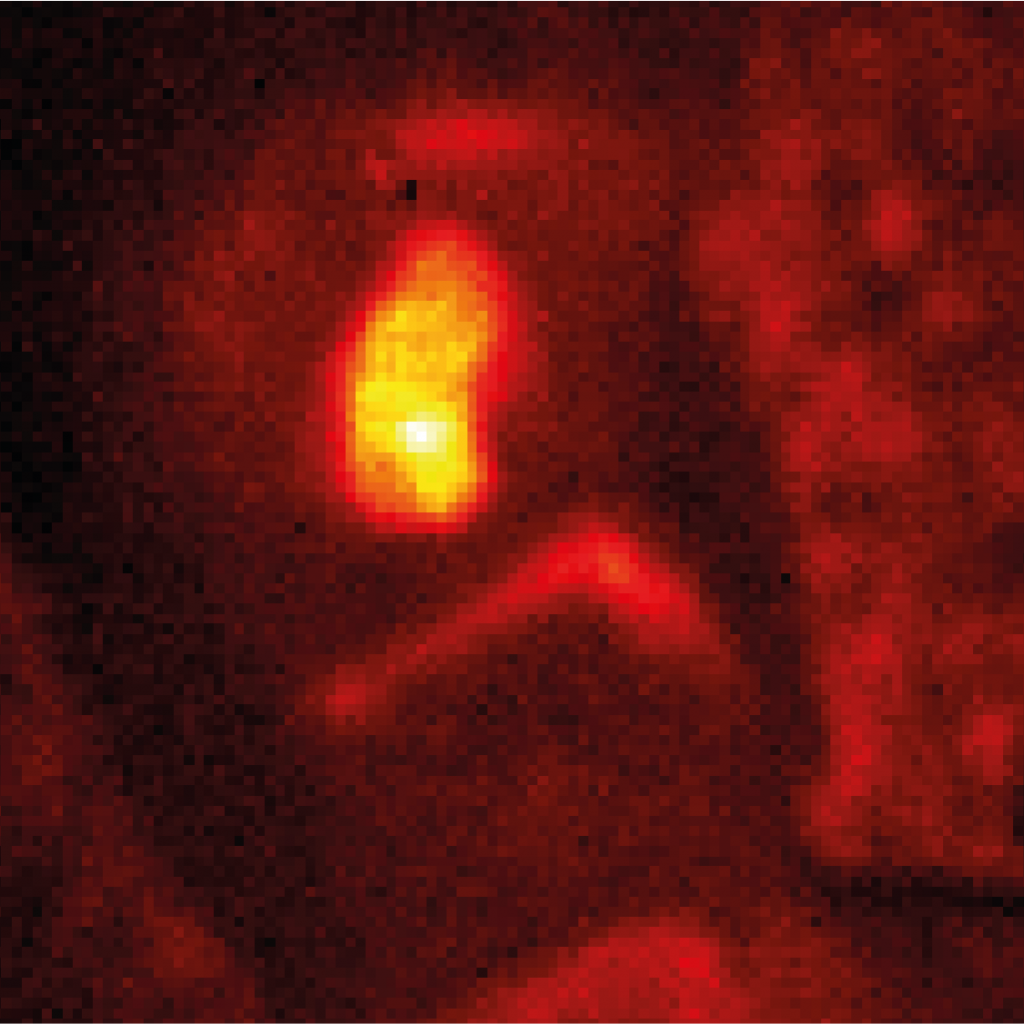
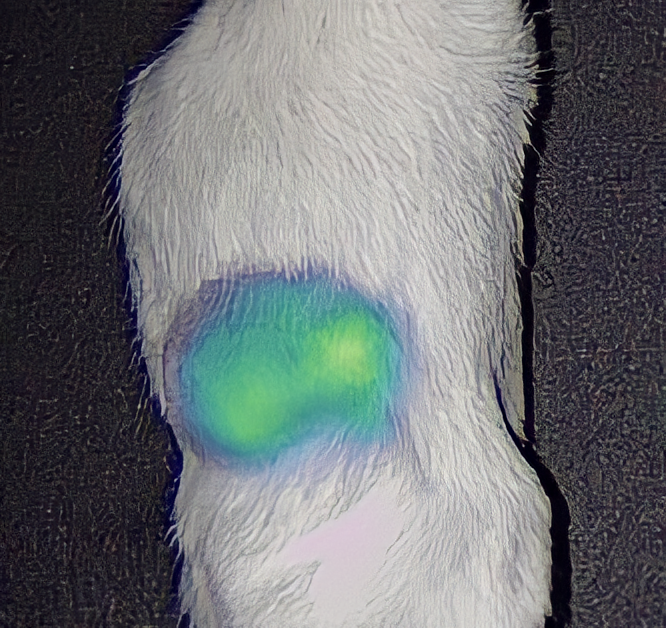
When these modified antibodies are introduced to the body, they attach to the neuroblastoma cells and nowhere else. This means that when the tumour is exposed during surgery, it is literally ‘lit up’ against surrounding tissue by all the fluorescent molecules attached to it. For surgeons, this makes it much easier to distinguish cancerous cells from healthy cells and remove the tumour accurately. High-resolution scanners can be used to detect any leftover cancer cells not visible to the naked eye, making surgery as comprehensive as possible.
Progress and next steps
“We have obtained good data in vitro and in animal models for this technique,” says Stefano. “We are about to submit an important paper to publish these results.” ‘In vitro’ refers to experiments not performed on living organisms, using cancer cells grown in the lab. Typically, this is the first step of testing new medical techniques, which precedes testing on animals, which precedes testing on humans. Once in vitro experiments had been completed, the team moved on to using FGS to remove neuroblastoma in mice. “Animal models are essential to obtain meaningful data before using the same technologies in humans,” says Stefano. “Now, the next step will be to translate our findings to humans in a clinical trial.”
The team hopes this new technology will be saving children’s lives within five years. “Surgery will be more precise, leaving less cancer behind and bringing benefits to rates of survival and recovery from surgery,” explains Stefano. “Patients will receive less extensive and more targeted surgery, with less risk of complications.” By removing the smallest parts of the tumours, it is expected that recurrence will be much reduced. In time, this technique could be extended to treat many different types of cancer, potentially saving many lives worldwide.
 DR STEFANO GIULIANI
DR STEFANO GIULIANI
Consultant Neonatal and Paediatric Surgeon at Great Ormond Street Hospital, Associate Professor at UCL Great Ormond
Street Institute of Child Health, Co-Investigator at the Wellcome/EPSRC Centre for Interventional and Surgical Sciences (WEISS), London, UK
Fields of research: Neonatal and Paediatric Surgery, Cancer Research
Research project: Using fluorescent antibodies to clearly distinguish tumours, allowing safer and more precise surgery for treatment of neuroblastoma in children
Funders: Medical Research Council (grant reference MR/T005491/1), Wellcome Trust-Innovator Award (grant reference 222111/Z/20/Z)
Wellcome/EPSRC Centre for Interventional and Surgical Sciences at University College London (WEISS, grant number 203145Z/16/Z), GOSHCC cancer infrastructure award
ABOUT NEONATAL AND PAEDIATRIC SURGERY
Neonatal and paediatric surgery involves surgery specific to babies and children. Often, the conditions they face, and the appropriate treatments, differ to those for adults, which has led to the development of these specialised fields. Like many medical professionals, the work of neonatal and paediatric surgeons like Stefano is typically split between treating patients and performing research.
“A particularly skilled professor of surgery inspired me when I was a medical student in Italy. His surgical skills, humanity and determination made me willing to pursue a career in academic surgery,” says Stefano. “I love my job, and I believe passion and dedication are essential to succeed in any career.”
The Great Ormond Street ICH is world-famous for leading the way in paediatric care, and Stefano’s work is contributing to this reputation. “One of my proudest achievements is having developed an independent research group on image-guided surgery,” he says. “This has been my dream for many years, and I obtained it with the support of ICH and my academic mentors, Professor Anderson and Professor De Coppi.”
Though there have been many advances in the field, both in terms of knowledge and technologies, Stefano believes there is a lot more progress to be made, presenting exciting opportunities for the next generation. “Paediatric and neonatal surgery is one of the most fascinating fields in medicine,” he says. “There is a lot to discover in complex fields such as foetal development, congenital anomalies, rare diseases and cancers.”
Reference
https://doi.org/10.33424/FUTURUM392
Pathway from school to neonatal and paediatric surgery
“A strong foundation in biology, mathematics and computing is essential for the medical careers of the future,” says Stefano. “Artificial intelligence, digital surgery and rapid pace innovations are increasingly driving forward medicine and biomedical research.”
“A strong background in biology is a must,” says Laura. “I would also encourage broadening your knowledge of statistics, chemistry and physics.”
“The lines between the traditional science subjects are becoming increasingly blurred,” says Dale. “Most challenges require expertise from multiple disciplines, so I would recommend taking a broad range of subjects. Learning maths and learning to code are becoming especially central to all scientific endeavours.”
Explore careers in neonatal and paediatric surgery
• Stefano recommends shadowing a paediatric surgeon to see whether you like the type of work they do, and then ask for research projects in the field. He suggests contacting a local academic paediatric surgeon to kickstart this process. The British Association of Paediatric Surgeons has a public directory.
• Dale emphasises the importance of communication for any area of science. He recommends learning to communicate with others, both within your area of expertise and those in the wider world. This podcast from THIS.Institute explains more.
• Laura points to PubMed as the go-to resource for researching specific medicine-related topics. She also recommends following blogs and watching webinars to keep up-to-date with the latest advancements in the field.
• UCL Great Ormond Street Institute of Child Health offers work experience, talks for medical students and engagement sessions with patients and parents. Find out more.
Meet the team
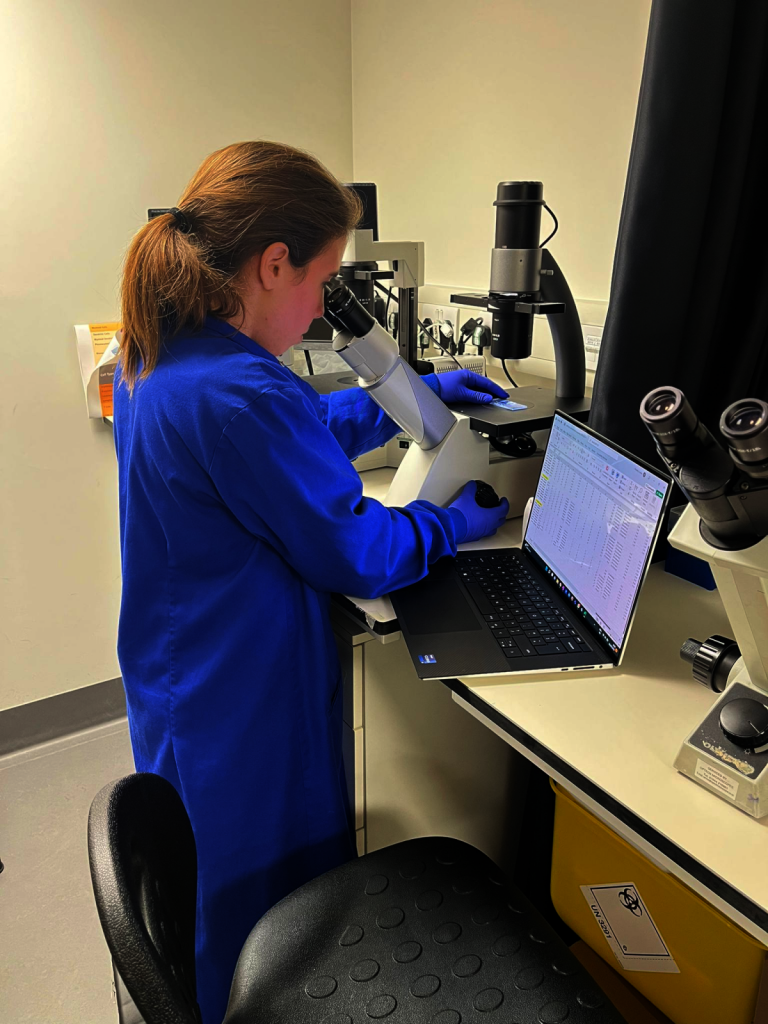
Dale and Laura both work in Stefano’s research group. They talk about their roles on the project and how their backgrounds led them to their current positions.

Dr Dale Waterhouse
Wellcome / EPSRC Centre for Interventional and Surgical Sciences (WEISS), London, UK
My role in the group is to help develop biomedical imaging devices (specialised cameras). Elsewhere, my biomedical imaging work leads to me contributing to research into neurosurgery, laparoscopic surgery and endoscopy.
I didn’t really enjoy science until I was in my final year of school. Around this time, scientists in Geneva were planning to switch on the newly constructed Large Hadron Collider; in my A-level science class there was an uncharacteristic buzz of excitement. My passion for science grew as I read popular science books. These revealed new realms of science – time travelling twins, evolutionary battlefields, warping fabrics of reality – concepts absent from the relatively dry school curriculum. From then, I knew I wanted to learn more.
I’ve tended to seek projects I enjoy and work with people I get along with, trust or admire. Following my degree, I applied for a prestigious PhD programme in particle physics, but I didn’t get a place. In retrospect, this was a fortuitous ‘failure’. It led me to a PhD position with a young, upcoming professor I respected and admired – in her lab, I found opportunities to grow and develop into a better scientist. For this, I am very thankful.
Research is time consuming, and things don’t always work as initially planned. I am constantly challenged to evolve my thinking and generate new approaches to solving problems. Sometimes these challenges are scientific, but often they are operational challenges like acquiring funding, troubleshooting equipment failures or finding a bug in my code.
Learning about a clinical challenge and then working with a team to generate bold new ideas is the most engaging part of my work. It takes many months, sometimes years, of hard work for these ideas to become reality, but when they finally do, it is very rewarding. The most rewarding is yet to come, when one day, hopefully, these advances make their way into routine care and change the lives of patients.
My proudest career achievement, so far, is when my PhD thesis was published as a book.
In the long term, I would like to be a professor of biomedical imaging, leading a multidisciplinary research team towards advancing surgical imaging techniques.
A typical day for me in three words? “That was unexpected!”

Dr Laura Privitera
UCL Great Ormond Street Institute of Child Health, Developmental Biology & Cancer Department, London, UK
Centre for Interventional and Surgical Sciences (WEISS), London, UK
I initially joined the group as a Clinical Research Fellow, and I have very recently embarked on a three-year PhD on image-guided surgery. I have only been working in this field for two years, so the biggest asset I bring to the group is my passion and determination.
During my final year at university, I had the amazing chance to work at the Great Ormond Street Hospital. It was the academic clinicians that I had the opportunity to work alongside during my internship that really inspired me to pursue a career in research. The people I worked with are internationally renowned, and this was an incredibly important opportunity for my personal and academic growth. I enjoyed the experience so much that I applied for a research position after graduating. I am only at the beginning of my research career, but I believe that what we are working on is truly ground-breaking.
In this line of work, you are challenged daily. There is always a new experiment or a new procedure to learn, and this can be both exciting and overwhelming at times!
Being part of a multidisciplinary team like ours has given me the opportunity to be involved with different projects that have resulted in publications and presentations at conferences. It has also been an exceptional opportunity to create new connections and expand my knowledge.
I am proud of being awarded the “Peter Paul Rickham prize for the best basic science paper” at the international congress of the British Association of Paediatric Surgeons (July 2022).
My ambition is to be an academic paediatric surgeon with a special focus on innovation in cancer surgery. I believe the field of surgical oncology will experience significant advances, and I want to be ready for this change.
The three words that describe a typical day for me are engaging, challenging and rewarding!
The team’s top tips
1. Try to pursue the things you love. If you don’t love it, you won’t spend time on it.
2. You will inevitably encounter obstacles and bad days along the way. Always keep in mind the end goal to never lose focus.
3. Study hard and dream big. You cannot do high quality research unless you are a dreamer.
Do you have a question for Stefano, Dale or Laura?
Write it in the comments box below and Stefano, Dale or Laura will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)