Making ill health in old age a thing of the past
Deborah Dunn-Walters is Professor of Immunology at the University of Surrey. Her research is focused on B cells and the role they play in the immune system, particularly as we age. The findings could lead to improved treatments that enable us to lead healthier lives for longer
It is therefore important to understand more about the key processes involved in immunity so that we can discover more about diseases such as these. However, this is easier said than done – the immune system is an extraordinarily complex network of special cells, proteins, tissues and organs, which all work together to protect us against infectious organisms and other substances.
Deborah Dunn-Walters is a professor of immunology at the University of Surrey, who leads a team focused on learning more about the immune system, particularly antibodies. One of the key questions her work seeks to answer is how the immune system changes in ageing.
Our immune system defends our body against invaders known as pathogens, such as viruses and bacteria. When an immune response is triggered, antibodies are produced, which bind to the pathogens and neutralise toxins. Other cells destroy the pathogens that have been tagged by antibodies.
Of course, this simple summary does not describe the full workings of our complex immune system; many other mechanisms are involved. For a more detailed description of how the immune system works, check out Kids Health: https://kidshealth.org/en/parents/immune.html
THE MEMORY OF THE IMMUNE SYSTEM
Once produced, antibodies stay in our bodies, allowing us to “remember” pathogens we have encountered before. Think about chicken pox; if you have had this disease then it is highly unlikely you will get it again. This is incredibly important because there have been instances throughout history, where no previous exposure to certain pathogens have led to widespread death and disease. In 1519, there were 22 million people in Mexico, none of whom had been exposed to European diseases. In March 1520, the Spanish fleet arrived and there was a smallpox epidemic soon after. Over 9 months, 8 million people died.
HOW DID DEBORAH COME TO BE INTERESTED IN THE BIOLOGICAL BASIS OF AGEING?
The biggest single risk factor for disease is age, which often means that the diseases and frailties associated with old age are something most people take for granted. Deborah’s interest in ageing began early in life as, being close to her grandparents, it seemed unfair that they should have so much zest for life and yet be prevented from doing what they wanted because of ill health. “During my PhD, I read papers that made me realise we don’t have to accept that old age is always accompanied by disability,” explains Deborah. “There may be biological mechanisms of ageing that can be treated in order to prevent disease.”
Since then, Deborah’s interest in the biological basis of ageing has grown. Understanding how to attain lifelong health has always been at the heart of what she does.
HOW HAS DEBORAH’S RESEARCH EVOLVED?
Early in her career, Deborah spent time performing cancer research. Cancers form when changes, called mutations, take place within the genes of a cell or a group of cells. Genes contain long strings of DNA, which act as coded messages telling the cell what to do. Therefore, in cancer, a gene mutation (a permanent alteration in our DNA) is generally considered a “bad thing”.
After moving to a lab that studied a cancer of B cells, however, Deborah discovered that the genes for antibodies undergo a deliberate process of mutation. “I found this absolutely amazing,” says Deborah. “DNA damage can be such a destructive process that kills cells or causes cancer, but our immune system has evolved a highly complex and regulated way of changing our DNA for the good.”
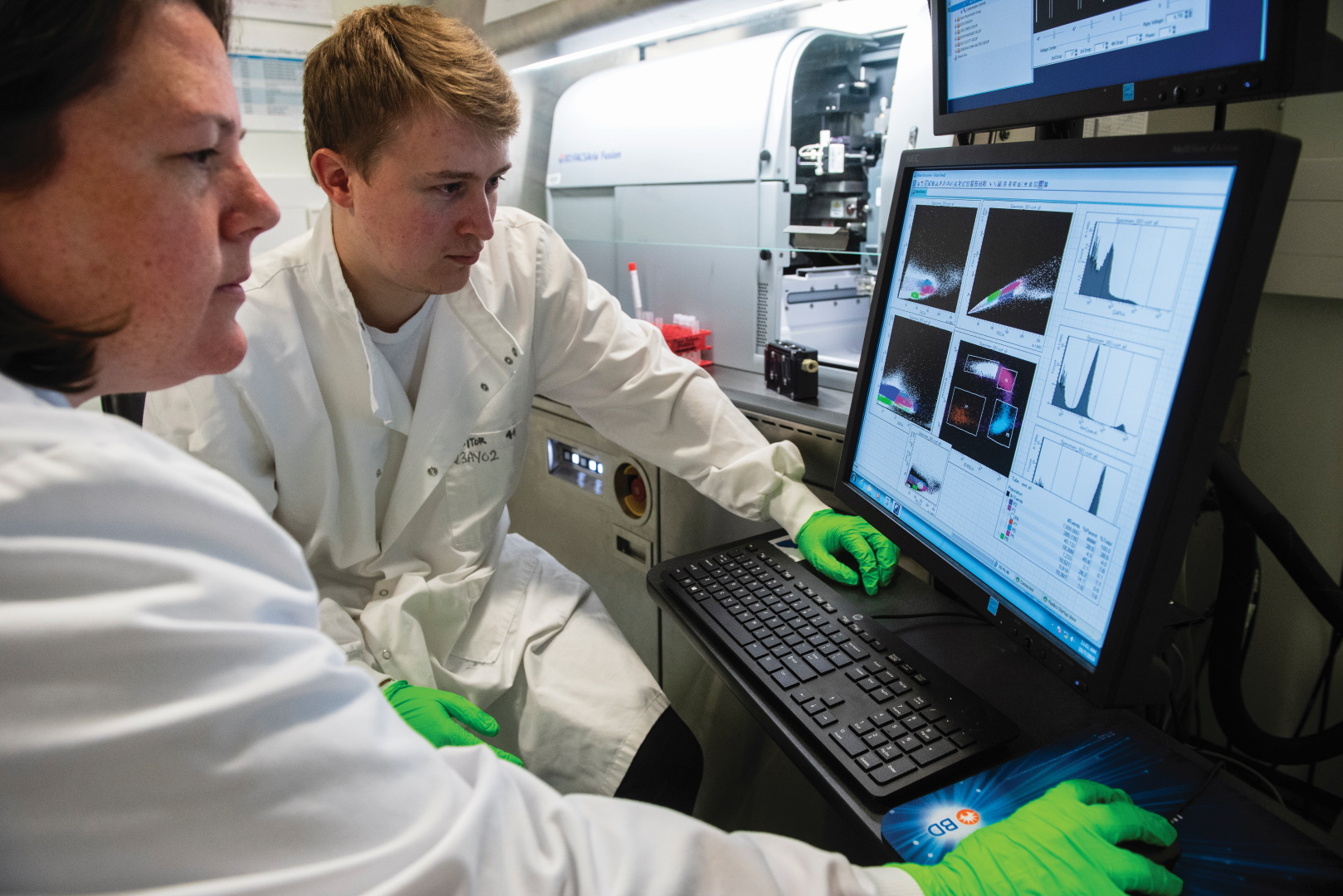
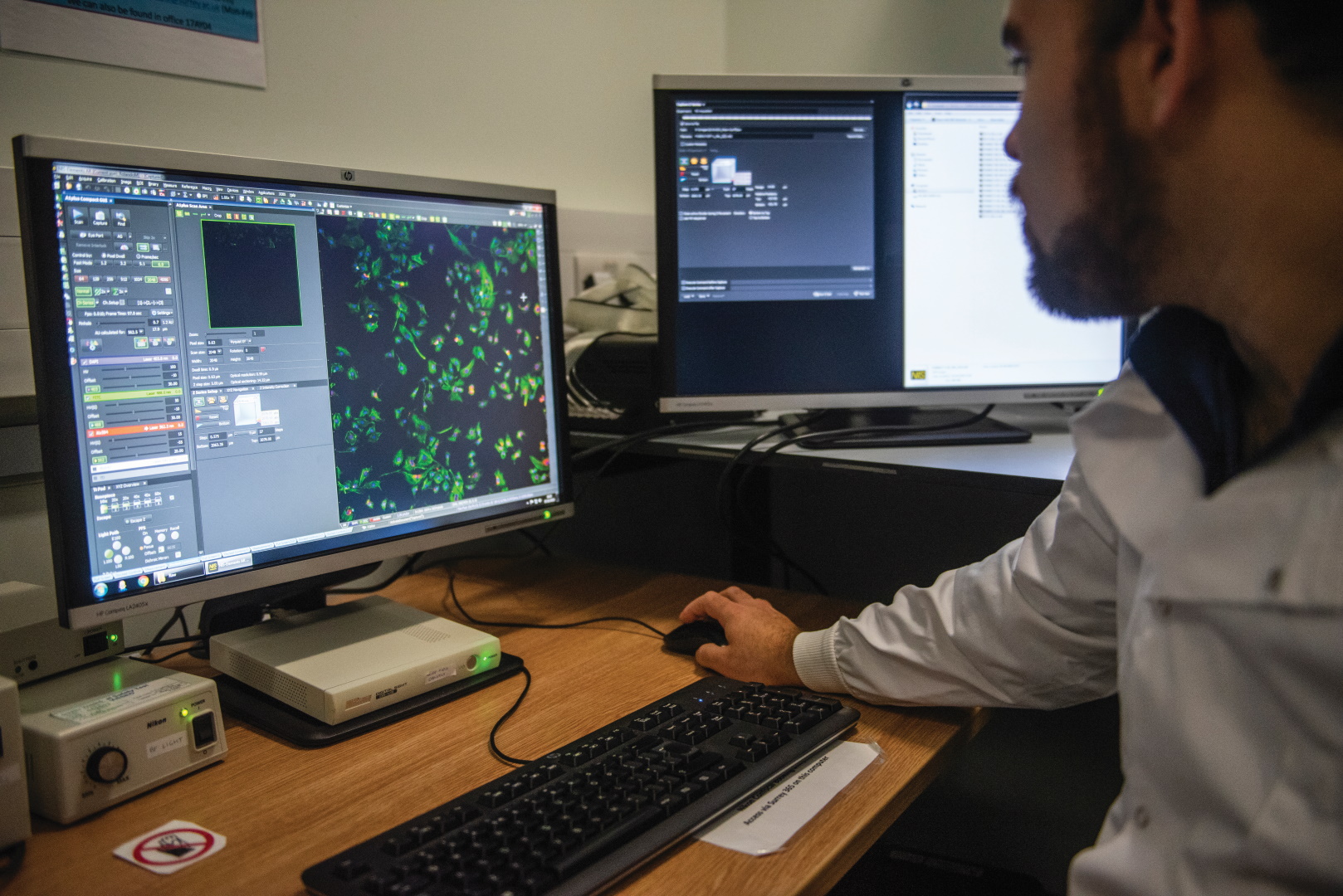
Deborah has been hooked ever since, and when it became possible to investigate an enormous number of antibody genes at a time, through a scientific process known as high throughput sequencing, she jumped at the chance to discover more. Since then, Deborah and her team have developed tools and understanding that have enabled many more scientists to look at the antibody repertoire in a wide variety of situations.
WHY ARE OLDER PEOPLE MORE SUSCEPTIBLE TO DISEASES SUCH AS RHEUMATOID ARTHRITIS?
Autoreactive antibodies are antibodies that bind to themselves instead of binding to invaders. There may be millions of different invaders we want our antibodies to bind to, and our bodies have a largely random method of making antibodies in order to achieve this. The flip side of this is that some of the antibodies we make might bind to our own molecules and cells.
Reference
https://doi.org/10.33424/FUTURUM31
It is therefore important to understand more about the key processes involved in immunity so that we can discover more about diseases such as these. However, this is easier said than done – the immune system is an extraordinarily complex network of special cells, proteins, tissues and organs, which all work together to protect us against infectious organisms and other substances.
Deborah Dunn-Walters is a professor of immunology at the University of Surrey, who leads a team focused on learning more about the immune system, particularly antibodies. One of the key questions her work seeks to answer is how the immune system changes in ageing.
Our immune system defends our body against invaders known as pathogens, such as viruses and bacteria. When an immune response is triggered, antibodies are produced, which bind to the pathogens and neutralise toxins. Other cells destroy the pathogens that have been tagged by antibodies.
Of course, this simple summary does not describe the full workings of our complex immune system; many other mechanisms are involved. For a more detailed description of how the immune system works, check out Kids Health: https://kidshealth.org/en/parents/immune.html
THE MEMORY OF THE IMMUNE SYSTEM
Once produced, antibodies stay in our bodies, allowing us to “remember” pathogens we have encountered before. Think about chicken pox; if you have had this disease then it is highly unlikely you will get it again. This is incredibly important because there have been instances throughout history, where no previous exposure to certain pathogens have led to widespread death and disease. In 1519, there were 22 million people in Mexico, none of whom had been exposed to European diseases. In March 1520, the Spanish fleet arrived and there was a smallpox epidemic soon after. Over 9 months, 8 million people died.
The biggest single risk factor for disease is age, which often means that the diseases and frailties associated with old age are something most people take for granted. Deborah’s interest in ageing began early in life as, being close to her grandparents, it seemed unfair that they should have so much zest for life and yet be prevented from doing what they wanted because of ill health. “During my PhD, I read papers that made me realise we don’t have to accept that old age is always accompanied by disability,” explains Deborah. “There may be biological mechanisms of ageing that can be treated in order to prevent disease.”
Since then, Deborah’s interest in the biological basis of ageing has grown. Understanding how to attain lifelong health has always been at the heart of what she does.
HOW HAS DEBORAH’S RESEARCH EVOLVED?
Early in her career, Deborah spent time performing cancer research. Cancers form when changes, called mutations, take place within the genes of a cell or a group of cells. Genes contain long strings of DNA, which act as coded messages telling the cell what to do. Therefore, in cancer, a gene mutation (a permanent alteration in our DNA) is generally considered a “bad thing”.
After moving to a lab that studied a cancer of B cells, however, Deborah discovered that the genes for antibodies undergo a deliberate process of mutation. “I found this absolutely amazing,” says Deborah. “DNA damage can be such a destructive process that kills cells or causes cancer, but our immune system has evolved a highly complex and regulated way of changing our DNA for the good.”
Deborah has been hooked ever since, and when it became possible to investigate an enormousnumber of antibody genes at a time, through a scientific process known as high throughput sequencing, she jumped at the chance to discover more. Since then, Deborah and her team have developed tools and understanding that have enabled many more scientists to look at the antibody repertoire in a wide variety of situations.
WHY ARE OLDER PEOPLE MORE SUSCEPTIBLE TO DISEASES SUCH AS RHEUMATOID ARTHRITIS?
Autoreactive antibodies are antibodies that bind to themselves instead of binding to invaders. There may be millions of different invaders we want our antibodies to bind to, and our bodies have a largely random method of making antibodies in order to achieve this. The flip side of this is that some of the antibodies we make might bind to our own molecules and cells.
WHAT ARE B CELLS?
B cells are a type of white blood cell that produce antibodies to fight infection and help other cells by presenting foreign antigens to them. Foreign antigens originate from outside our bodies and are parts of, or substances produced by, viruses or bacteria; other examples of foreign antigens include bee venom or certain proteins in food.
Deborah and her team have shown that levels of a particular type of B cell are reduced in older people. They believe that this type of cell is very important in making antibodies that bind to the types of antigens that you find on the surface of bacteria, such as those that cause urinary tract infections and pneumonia. However, it is worth noting that there are many other different types of cells in the immune system that are also important for the body’s defence, so there is still a lot to discover.
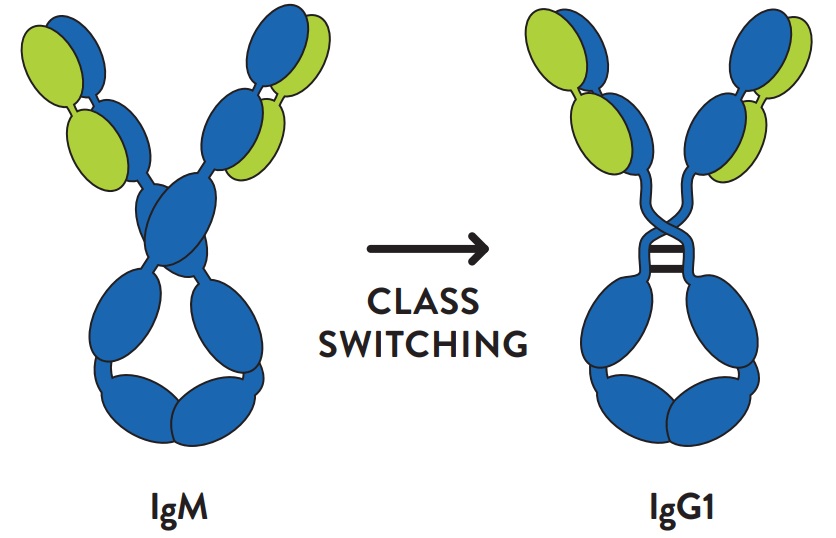
Class switching from Immunoglobulin M (the largest antibody known as IgM) to Immunoglobulin G1 (IgG1), a subtype of Immunoglobulin G, which is the most abundant antibody in the human blood. This class switching enables binding on a phagocyte. A receptor is a protein that binds to a specific molecule. Phagocytic cells are cells that can engulf and destroy
UNDERSTANDING IMMUNOLOGY AT A HIGHER LEVEL
SPECIFICITY – a set of characteristics or behaviours that are specific to a living organism or part of the living organism
MODEL – a physical, conceptual or mathematical representation of a real phenomenon that is difficult to observe or experiment on.
ANTIBODY REPERTOIRE – an inventory of all the different kinds of antibody in the immune system.
Deborah’s team has reached the conclusion that the mechanisms that produce a diversity of antibodies do not change much with age, but the mechanisms in the immune system that select which antibodies survive and which are amplified do differ with age. “We have highlighted the importance of a certain part of the antibody for the specificity of target binding [e.g. binding to invaders],” says Deborah. “We also have models showing that one antibody may bind to a number of different targets, and the ratio of self to non-self binding in the repertoire can affect how well the system can react to protect us against infection.”
In addition, the team has shown that antibodies with different functional regions may be more important than we think. An antibody can have the same specificity for a target but can change what it does when it binds by switching the functional half of itself to a different class of antibody. So, one class of antibody may just bind and block a target, but another might bind the target and signal to another cell to come and destroy it. This is known as class switching.
 DEBORAH DUNN-WALTERS
DEBORAH DUNN-WALTERSProfessor of Immunology
University Champion for Lifelong Health Research Theme, University of Surrey, UK
FIELD OF RESEARCH: Immunology
RESEARCH PROJECT: Deborah focuses her research on B cells and the role a particular type of B cell plays in immune system changes in ageing. The findings could shape our understanding of what happens to us as we age and lead to improved drug
treatments.
FUNDERS: Dunhill Medical Trust; Medical Research Council; The Biotechnology and Biological Sciences Research Council; The Rosetrees Trust; Medimmune; Human Frontiers Science Program
 DEBORAH DUNN-WALTERS
DEBORAH DUNN-WALTERSProfessor of Immunology
University Champion for Lifelong Health Research Theme, University of Surrey, UK
FIELD OF RESEARCH: Immunology
RESEARCH PROJECT: Deborah focuses her research on B cells and the role a particular type of B cell plays in immune system changes in ageing. The findings could shape our understanding of what happens to us as we age and lead to improved drug
treatments.
FUNDERS: Dunhill Medical Trust; Medical Research Council; The Biotechnology and Biological Sciences Research Council; The Rosetrees Trust; Medimmune; Human Frontiers Science Program
ABOUT IMMUNOLOGY
Immunology is the study of the immune system. Given the importance of the immune system, it is hardly surprising that it is an extremely important branch of the medical and biological sciences. If the immune system is not functioning as it should, there can be a range of problems, such as disease, autoimmunity and allergies. The more scientists study immunology, the more they learn about the complexities and intricacies of immune responses. In recent times, it has become clear that responses of the immune system can contribute to the development of a wide range of common disorders that were previously thought to have no relation to immunology, such as cardiovascular and neurodegenerative conditions.
WHAT ABOUT VACCINES?
Perhaps the clearest, most obvious example of immunology at work is found in vaccinations. In 1796, Edward Jenner carried out an experiment on an 8-year-old called James Phipps. Jenner put pus taken from a cowpox pustule into an incision on James’ arm. He did this to test his theory that milkmaids who suffered the relatively mild cowpox disease never contracted smallpox. James was unscathed, became immune to smallpox, and Jenner had proved it was possible to inoculate people from the smallpox virus by exposing them to cowpox.
The vaccine was born and so too was the field of immunology. It is impossible to know how many lives Jenner has saved with his experiment, but, according to Our World in Data, reasonable estimates put the figure at between 150 and 200 million lives between 1980 and 2018, alone.
WHAT IS AN IMMUNOLOGIST?
An immunologist, like Professor Deborah Dunn-Walters, is a scientist or clinician who specialises in immunology. Many immunologists work in laboratories around the world to improve our understanding of the immune system. And some work on immunotherapy to combat diseases such as cancer, or decide to focus on the diagnosis and management of diseases of the immune system, such as autoimmune diseases and allergies.
OPPORTUNITIES IN IMMUNOLOGY
• The British Society for Immunology has dedicated an area of its website to careers, where you can find a variety of options concerning the study of immunology at different degree levels.
• There are so many different branches in the field of immunology that determining an average salary is difficult. However, prospects.ac.uk says it is typical for clinical scientists working in the UK National Health Service (NHS) and training in immunology to earn around £28,000, rising to over £100,000 for those working at the very highest level.
• Immunologists work in a broad range of roles, such as biochemists, microbiologists, toxicologists and medicinal chemists. It really depends on whether you want to be part of the research, discovery or phased trials aspect of the sector.
ASK PROF DEBORAH DUNN-WALTERS
WHAT DID YOU WANT TO BE WHEN YOU WERE YOUNGER?
At school I cycled through lots of different options. I wasn’t big enough to be a firefighter! I thought about pharmacy for quite a long time, then marine biology because the underwater world fascinates me. I ended up enrolling for a chemistry degree because I thought the post-study employment options would be good. Fortunately, in the first year we did as much biology as chemistry, so I could switch to biology when I realised that: a) I enjoyed biology much more, and b) I didn’t have a very good memory; and if I couldn’t even memorise the periodic table then chemistry was going to make me miserable!
WHAT FASCINATES YOU MOST ABOUT IMMUNOLOGY AND THE AGEING PROCESS?
The most fascinating aspect for me is how the complexity of different cells, the chemical signals between cells, and the environments that support the cells hang together to give us a near perfect protection against attack from the microbial world or dangers from within. Much of the time our immune system is acting to protect us, and we don’t even notice. We have only scratched the surface in terms of understanding – I am not at all surprised it starts failing in old age – I am more surprised it works as well as it does for as long as it does. We just need to figure out what fails to know how to help it.
WE ARE LIVING LONGER, BUT FROM AGE 60 ONWARDS, WE EXPERIENCE AN AVERAGE OF 19 YEARS IN POOR HEALTH. DO YOU THINK SCIENCE WILL EVENTUALLY FIND AN ANSWER TO LIVING LONGER IN GOOD HEALTH?
Science has already discovered some ways to reduce the amount of time we live in poor health. Unfortunately, we don’t yet have tablets you can take once you are old – you need to live your life up to that age taking adequate exercise, eating healthy foods, not drinking too much alcohol and not smoking. Keeping healthy is a lifelong thing and until science comes up with magic pills, we need to try a little bit harder to live our lives better. Think of it like saving up for a pension: the more good health you bank now, the more you will have later.
HAS YOUR RESEARCH INFLUENCED THE WAY YOU LEAD YOUR LIFE?
I do try to live a healthy life, but I don’t go to extremes. You won’t find me doing triathlons or practising extreme calorie restriction, but I do enjoy hiking, gardening, DIY and swimming, and I steer towards fresh fruit and veg in the supermarket.
01 If you are interested in a career in immunology, you should certainly study biology before you go to university – although chemistry is useful, too.
02 You will need a degree to become an immunologist, so take degree courses in biosciences that include immunology modules at university. Some people go further and take an MSc in immunology to supplement their degree knowledge.
03 Don’t be afraid to take other subjects along the way if they grab your interest. It is always possible you might change your mind, so take subjects you are passionate about. We all have long working lives and it is very important that we enjoy our jobs!