What do we know about the ovary?
Ovarian cancer ranks fifth in cancer deaths amongst women, with a woman’s risk of getting it during her lifetime being about 1 in 78. Polycystic ovary syndrome (PCOS) is the most common endocrine and ovulation disorder in women that severely alters fertility. At Baylor College of Medicine in Texas in the US, Professor JoAnne S. Richards has dedicated her career to improving our knowledge and understanding of the ovaries, with the ultimate hope of improving women’s health worldwide.
TALK LIKE A MOLECULAR AND CELLULAR BIOLOGIST
Embryo — an unborn, developing offspring. In humans, the embryonic stage lasts from approximately the second to eighth week after fertilisation
Gamete cell — the reproductive female or male germ cell
Membrane — a thin sheet of extracellular matrix protein or layer of cells that act as a boundary or lining between specific cell types
Metastatic cancer — a dangerous, late stage of cancer where it spreads to distant parts of the body
Omentum — fatty tissue in the peritoneal cavity
Ovary — an endocrine gland at the upper end of the uterus that contains follicles and corpora lutea, the sources of steroid hormones, and releases mature oocytes (eggs) at the time of ovulation
Ovulation — the process during which an egg surrounded by specialised cumulus cells is released from the surface of the ovary for fertilisation to occur
Peptides — compounds consisting of two or more amino acids linked in a chain, which can bind to specific receptors to alter cell functions
Pituitary gland — a pea-sized gland at the base of the brain that produces several protein hormones, including FSH and LH
Somatic cells — any cell in the body other than the gamete cells (sperm and egg cells)
Uterine — relating to the uterus
The ovary is an essential organ that plays a crucial role in the reproductive system of females. Professor JoAnne S. Richards, a molecular and cellular biologist at Baylor College of Medicine, has been studying the ovary for decades, learning about its various critical functions, as well as the causes of female infertility and ovarian cancer.
Females have two ovaries each, which are about the size of a thumb and are attached to the uterus located in the pelvic cavity. Ovaries contain the female reproductive cells, oocytes (eggs), which, once fertilised by a male sperm, can develop into a living embryo. Individual oocytes are one of the largest cells in the human body, measuring around 0.1 mm in size. Once grown, they are even visible to the naked eye.
“The primary functions of the ovary are to promote the maturation, ovulation and fertilisation of the oocyte and to regulate embryo implantation and uterine maintenance during pregnancy,” says JoAnne.
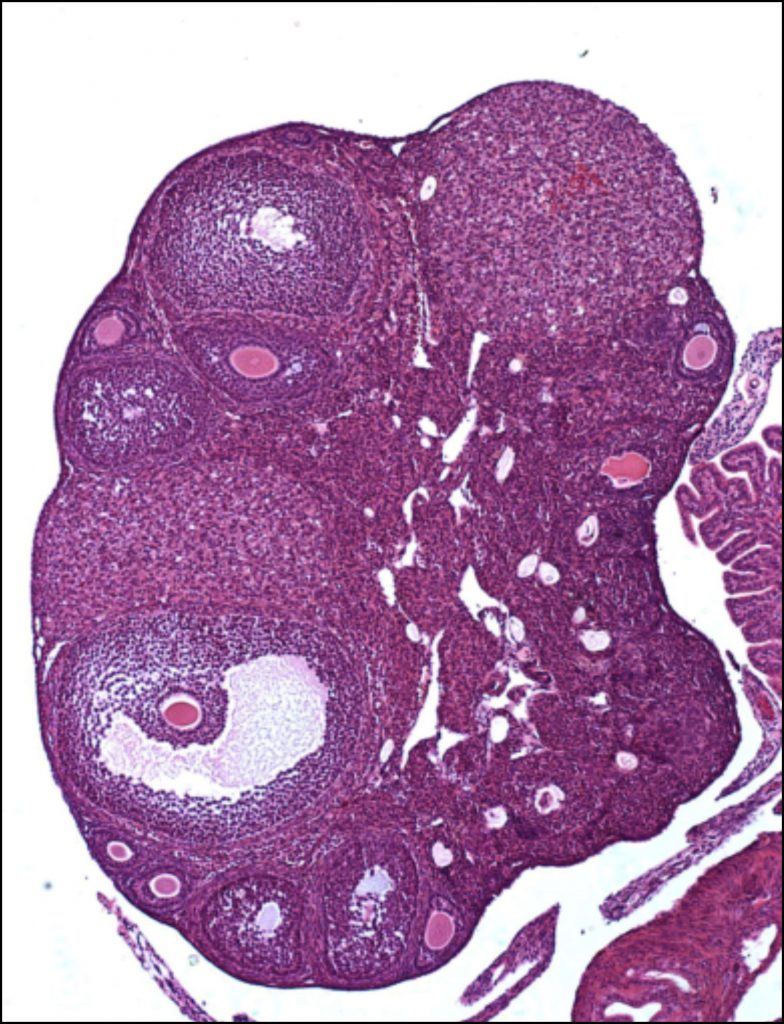
The ovary is controlled by two pituitary hormones called follicle stimulating hormone (FSH) and luteinising hormone (LH). These hormones act via receptors on specific cells to regulate the growth of ovarian follicles and the maturation of oocytes within these follicles. A surge of LH induces ovulation, during which a follicle ruptures and releases a mature, fertilisable egg.
What are follicles?
Ovaries contain thousands of follicles (all at different stages of development) that function to ensure that the oocyte is well-protected and nurtured, so it can mature and be fertilised.
“Inside a follicle, the oocyte is attached directly to special somatic cells called cumulus cells,” says JoAnne. “These cells come from the surrounding granulosa cell layer. FSH-responsive granulosa cells are then separated from LH-responsive theca cells (the outer cells) by a basement membrane.”
“The oocyte affects these somatic cells by releasing specific peptides. The somatic cells (granulosa and theca cells, in turn) coordinate and promote maturation of the oocyte,” JoAnne explains.
In addition, the somatic cells produce steroid hormones – oestradiol and progesterone, the major female sex hormones – that regulate embryo attachment and development during pregnancy. These steroids also control breast development and lactation, ensuring that mothers are able to breastfeed once they give birth (though other issues can make this difficult to do in practice, and not everyone chooses to breastfeed).
What do scientists know about the causes of female infertility?
“Age is a major factor in fertility,” says JoAnne. This is because women are born with all the oocytes they will ever have and are not able to make any more during their lifetime. “The ovary of a human infant immediately prior to birth contains around 6 million oocytes,” says JoAnne. “This number declines to around 1 million at birth; 300,000 at puberty; 25,000 at age 36 and about 1,000 at menopause. Thus, if women delay childbirth until age 40, they have difficulty conceiving.”
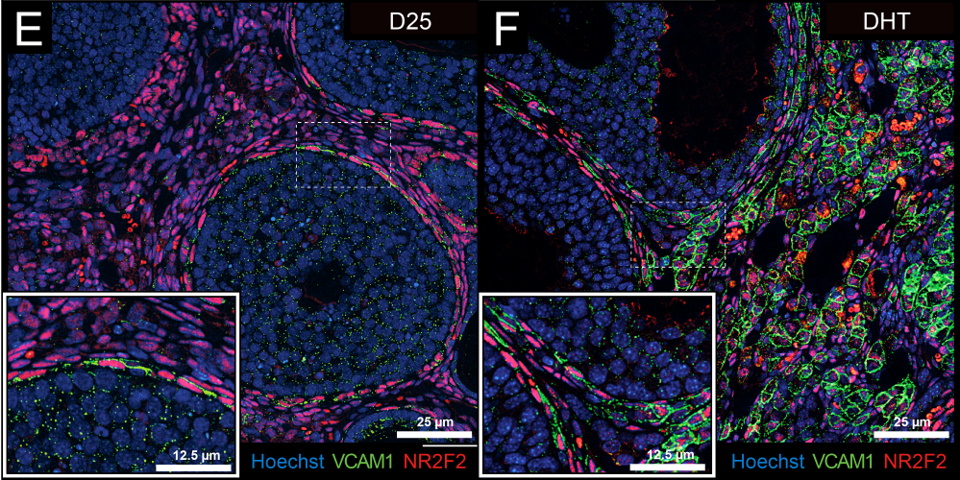
Women who have difficulty conceiving might consider in vitro fertilisation, also known as IVF. “IVF clinics can sometimes rescue ovulation,” says JoAnne. However, the number of follicles present and that can be stimulated to ovulate is greatly reduced, meaning the chances of getting pregnant through IVF at age 40 or later are much lower. There are multiple other causes of female infertility that scientists know about. Polycystic ovary syndrome (PCOS) is a common but complex cause that is associated with elevated levels of androgens, LH and obesity. “Women with PCOS can usually be stimulated to ovulate by managing levels of FSH and LH,” says JoAnne.
What do scientists know about ovarian cancer?
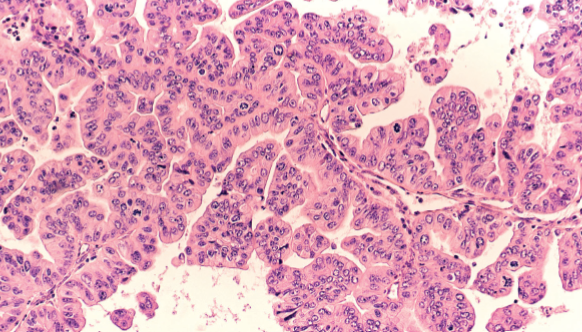
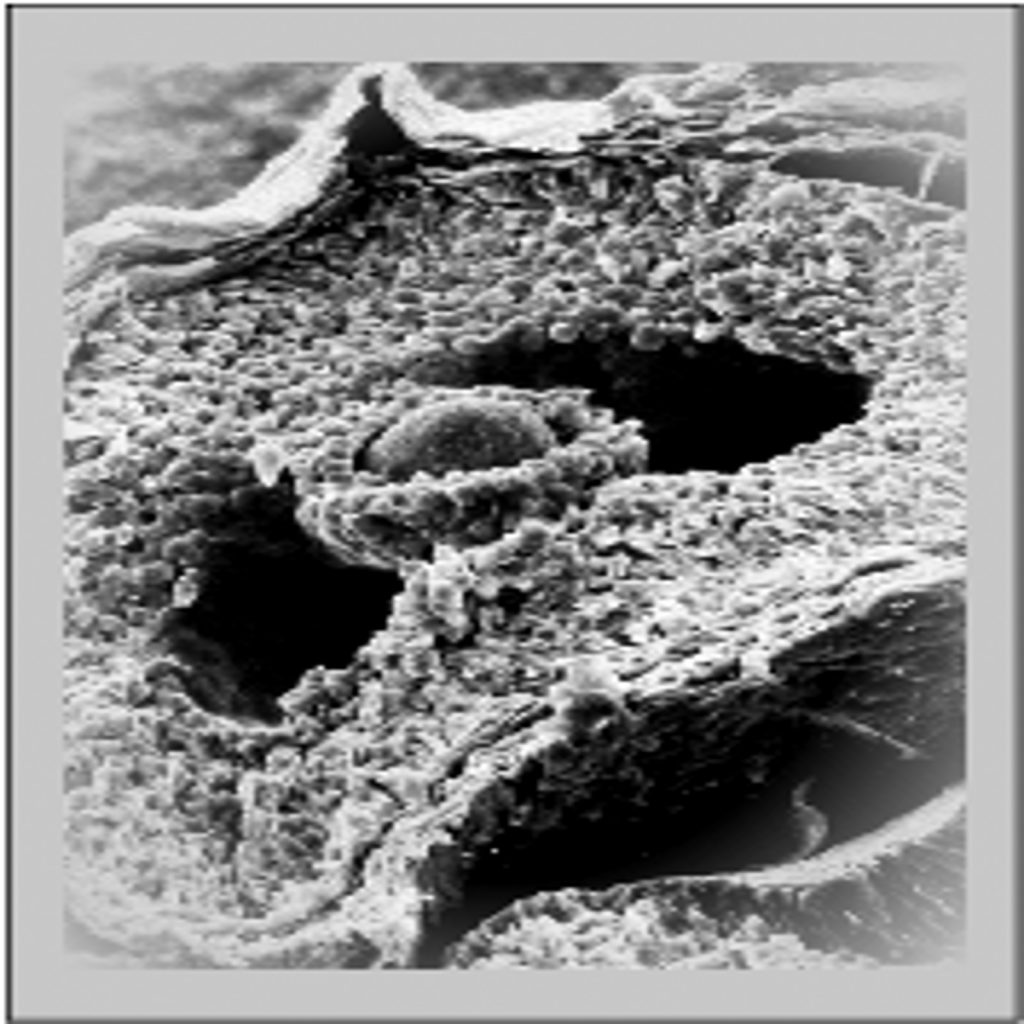
Unfortunately, ovarian cancer is a dangerous and deadly disease, with a survival rate of only 30% if diagnosed at an advanced stage. “The lethality of ovarian cancer is largely due to the late stage at which it is diagnosed and the extreme difficulty in removing the tumours surgically,” explains JoAnne. Current anticancer drugs are also only effective for short durations, as cancer cells have powerful mechanisms that allow them to become drug-resistant and evade cell death.
While there are multiple cells in the ovarian follicles that are helpful for the oocyte – such as the granulosa, theca and cumulus cells – there are some outside the follicles that can be dangerous. “Ovarian surface epithelial (OSE) cells, for instance, are not part of the ovulatory follicle and can give rise to ovarian cancer,” says JoAnne. Ovarian cancer can be caused by these OSE cells or by cancerous cells coming from the fallopian tubes that spread to the ovary and the omentum within the peritoneal cavity.
“The initial causes of ovarian cancer, as with other types of cancer, remain largely unknown,” says JoAnne. “99% of the time, ovarian cancer is associated with mutations in the tumour protein p53,” says JoAnne. p53 plays a role in DNA repair mechanisms, which means that mutations in p53 can prevent DNA from repairing itself, making cells more susceptible to damage and further mutations. Unfortunately, mutations in this and other genes can be passed down from parents to children, meaning that ovarian cancer can be an inherited disease.
Reference
https://doi.org/10.33424/FUTURUM371
A micrograph of a cancerous tumour in the female ovary.
(© David A Litman / shutterstock.com)
Candelaria et al: Endocrinology 160:1377-1393, 2019
What research has JoAnne done on ovarian cancer?
Some of JoAnne’s research has involved expressing KRAS – a gene that if mutated has been associated with cancer cell functions – in granulosa cells in mice. “When we did this, we saw that KRAS blocked follicle growth, reduced ovarian steroid production, and led to an increase in the tumour suppressor gene, PTEN,” says JoAnne. JoAnne and colleagues then disrupted expression of PTEN in the KRAS mutant mouse ovarian cells. “When we did this, follicle development remained blocked, but OSE cells (which can cause ovarian cancer) were transformed,” explains JoAnne. This provided one of the first mouse models of ovarian cancer.
After this, JoAnne and colleagues decided to reduce the p53 gene in the OSE cells of mutant mice. This led to the discovery that p53 was essential for tumour growth. “Cells lacking p53 developed only small tumour lesions that were exquisitely sensitive to steroid hormones and became highly metastatic when exposed to oestradiol,” JoAnne explains.*
The realisation that steroid hormones can impact some types of ovarian cancer might allow better treatments for this disease to be discovered in the future.
*a. Fan et al. Cancer Res. 69:6463-6472., 2009
- Mullany et al. Mol Endocrinol 28: 127-137 2014
 Professor Joanne S. Richards
Professor Joanne S. Richards
Department of Molecular and Cellular Biology, Baylor College of Medicine, Houston, Texas, USA
Field of research: Molecular and Cellular Biology
Research project: Studying ovarian function and related dysfunctions, such as polycystic ovary syndrome and ovarian cancer
Funder: National Institutes of Health (NIH)
About Molecular and Cellular Biology
Molecular and cellular biologists study the processes and interactions of cells and molecules in animals, microorganisms and plants. They will often work in lab environments, set up experiments, teach and write scientific papers to explain their findings to others. They can have wide-ranging impacts on other researchers as their work can advance various fields such as medicine, pharmaceuticals, food and agriculture.
Molecular and cellular biologists must love discovering the unknown, as working as a researcher will lead to lots of unexpected discoveries! “Science is a mindset, and I think one either has it or not,” says JoAnne. “It is not about making money. Rather, it is about people and the hope and joy of discovery. It is the ideas and puzzles of nature that provide the rewards and inspiration in science, with the ultimate hope of improving health for everyone.”
How has JoAnne contributed to scientists’ knowledge of ovarian function?
One of JoAnne’s biggest contributions was the discovery of a second form of the enzyme cyclooxygenase, now known as prostaglandin synthase-2 (PTGS2). This form is essential for ovulation and is selectively expressed by ovulating follicles.
“Prior to 1991, the scientific community only recognised a single cyclooxygenase gene,” says JoAnne. “My laboratory unexpectedly unveiled the second form, which is induced in ovulatory follicles by the luteinising hormone (LH). This was perhaps the most memorable moment in my career, because it was so unexpected, and it took us so long to figure it out!” *
What research opportunities will be open to the next generation of molecular and cellular biologists?
“The technologies available to molecular biologists are changing and expanding at a rapid pace. Analysing cells and genes at a single-cell level is the most recent approach. Microscopic technologies are also improving, becoming more powerful and being linked to computer driven images. Gene editing is now becoming routine, but this will face challenges of ethics. My hope is that we do not forget to see the big picture and understand the physiology and the beauty of the basic biology.”
* Wong and Richards Mol. Endocrinol. 5: 1269-1279, 1991.
Pathway from school to molecular and cellular biology
• At school and post-16, take as many science classes as you can. You will then need to complete an undergraduate degree in a scientific subject, such as biology, molecular biology, biophysics or biochemistry. After that, complete a master’s degree and a PhD in molecular biology.
• JoAnne recommends you also learn computer language skills, as well as English and writing skills.
• Before you choose a university, have a thorough look at their website to get an idea of their strengths.
• “Many institutions also have outstanding summer programmes,” says JoAnne. “For example, Baylor College of Medicine has a summer SMART (Summer Medical and Research Training) Program.”
• “Scientists must have a love of adventure and be willing to take failure,” says JoAnne. Something to keep in mind whichever route your pathway from school takes.
Explore careers in molecular and cellular biology
• “Working in a lab, almost any lab, is a great way to get started,” says JoAnne. Try and find workplace experience as soon as possible to see if a career in molecular and cellular biology is something you are truly interested in. You can also reach out to current biologists to see if they might have opportunities for you to shadow their work.
• The University of California Berkeley has a useful webpage summarising career options for people with molecular and cell biology degrees: mcb.berkeley.edu/undergrad/major/career
• The American Society for Cell Biology has a wealth of information on its website, including its Pathways Podcast series for those interested in life sciences.
• The British Society for Cell Biology also provides careers information.
• Salaries vary depending on position, employer (for example, you could work in academia or industry) and experience. CareerExplorer explains that a starting level molecular biologist can earn around $48,000 a year, while a senior molecular biologist could be earning around $133,000 a year.
Q&A
Meet JoAnne
What prompted your shift from majoring in French to pursuing a career in science?
My goal to become a French major changed in my second year of college when I had difficulty using headphones to distinguish recorded French conversation (little did I know that I had a hearing problem). Luckily, I was taking all the pre-med biology courses because I was keenly interested in biology, and eventually biology became my major.
Afterwards, I went to graduate school at Brown University to become a high school biology teacher. I learned the first day of practising teaching that this was not my calling – I had absolutely no disciplinary powers whatsoever! Luckily, the programme required a research experience and that evolved into my applying for the PhD programme in physiological chemistry (biochemistry) at Brown. This was my first exposure to research. Research in the ovary, with a focus on steroidogenesis, isolating steroid hormones was a big thing in the late 1960s. It was an exciting time!*
* Richards, JS. Discovering science and the ovary: a career of joy. Reproduction 158: F69-F80, 2019.
What do you find rewarding about research in your field?
What captures me most about science is the process of discovery and the challenges to decipher the secrets of Mother Nature. Most rewarding has been the unexpected experimental results that have led me down new paths and reminded me that one should always keep an open mind. In my lab, the most rewarding moments have been identifying a new cyclooxygenase gene, generating an unexpected mouse model of ovarian cancer, identifying novel pathways regulating ovulation and documenting a novel role for androgens in theca/stromal cells. In these discoveries, I have enjoyed the enthusiasm of young students and colleagues.
Scientists are rewarded by discovering new pathways, genes and approaches to understand biological processes. I have been richly rewarded throughout my career. None of this would be possible without the support of the Society for the Study of Reproduction, the Endocrine Society and the National Institutes of Health. These organisations, and the wonderful, dedicated people who maintain these scientific and educational opportunities and the yearly NIH sponsored, Frontiers in Reproduction, course at Woods Hole, Massachusetts, are the ones who sustain our research in endocrinology and reproductive biology.
What keeps you motivated as a scientist?
The most important motivator is the research itself: the ideas, the data, tackling new approaches to understand complex biological events. It is just so exciting to see novel data begin to unravel the current puzzle. There is nothing quite like having a complex experiment work.
I have also been motivated by my colleagues, students, other scientists and the camaraderie we have shared. The scientific excellence of the facilities and faculty at the University of Michigan and Baylor College of Medicine have motivated me, as have the scientific meetings around the world, which have brought new insights at all levels. Science is a world community that is open-minded. I have collaborators that I have never met, and have been lucky to work with a bright, energetic and thoughtful group of colleagues during my career.
JoAnne’s top tips
1. Don’t be afraid to see an experiment fail, seek help, ask questions. If failure was not due to technical issues, then there is something new to learn.
2. Enjoy tackling the unknown and love what you do. Perseverance is the key. If you like what you are doing, you will be successful.
3. Don’t let anyone take you for granted!
Do you have a question for JoAnne?
Write it in the comments box below and JoAnne will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)