Empowering people through health education
To make informed decisions about our own healthcare, we need to understand how our bodies work and the illnesses that can affect them. Unfortunately, diseases can be complicated, and information about them is not always clear or accessible. Dr Susan Creary is a paediatrician from the Hematology, Oncology and Blood and Marrow Transplant (BMT) Clinic at Nationwide Children’s Hospital in Columbus, USA. She and her team have created an education programme to spread awareness and understanding of sickle cell trait and what it means for individuals and families who inherit it.
Talk like a paediatrician
Health literacy — a person’s ability to find, understand and use information relating to their health, to make informed health decisions
Haemoglobin — a protein inside red blood cells that carries and delivers oxygen around the body
Inherited — in biology, things that are encoded in your body and that make you uniquely you. Inherited traits are passed from parents to children by genes
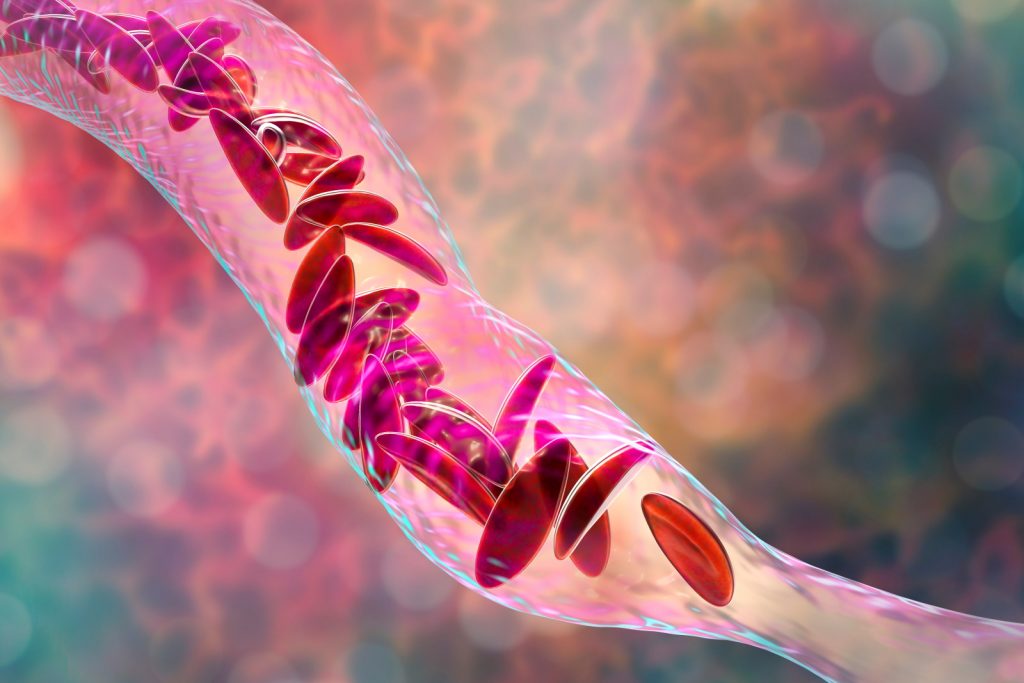
Sickle cell disease — an inherited disease that changes the shape of red blood cells. Red blood cells in someone with sickle cell disease are more likely to get stuck in their blood vessels and are not able to carry and deliver oxygen as they should. It is caused by inheriting sickle cell trait from both parents or sickle cell trait from one parent and another abnormal haemoglobin trait from the other parent
Sickle cell trait — an inherited trait but not a disease. It is caused by inheriting a sickle cell trait from one parent but a regular haemoglobin trait from the other parent. Individuals with sickle cell trait are not likely to suffer any symptoms but can still pass this trait on to their children
The human body is an incredibly complex collection of trillions of cells, proteins, molecules and microbes that are all connected. It is not surprising that when we become ill, it can be a puzzle to understand what has gone wrong and how best to fix it.
Luckily for us, we have medical researchers, doctors and nurses who train for years to understand how the human body works, why things go wrong and how to help us when they do.
It is important, however, that we also understand what is going on inside our bodies, so that we can keep ourselves as healthy as possible. For example, people with diabetes need to know how the disease works so they can maintain and monitor their blood sugar levels. If a patient does not have access to the right information, they are less able to take care of their own health.
Dr Susan Creary is a researcher at the Hematology, Oncology and Blood and Marrow Transplant (BMT) Clinic at Nationwide Children’s Hospital. Her research focuses on increasing knowledge and awareness of sickle cell trait. Sickle cell trait makes people at risk of having children with sickle cell disease. Dr Creary explains, “My aim is to deliver health information in a way that anyone, with any level of health literacy, can understand it and use that information to make decisions about their health.”
What is sickle cell disease?
Sickle cell disease is a condition that changes the shape of red blood cells. Healthy red blood cells are flexible and round, allowing them to easily move through our blood vessels and carry oxygen around our body. The blood cells of people with sickle cell disease become rigid and C-shaped like a sickle (an old farming tool). These C-shaped blood cells get stuck in blood vessels, preventing oxygen from being delivered to parts of the body as it should. This can lead to many complications, including intense pain and being at risk of certain infections.
What causes sickle cell disease?
Haemoglobin is a molecule that is inside red blood cells and carries oxygen. Sickle cell disease is a genetic condition that affects haemoglobin. Sickle cell disease happens when you inherit a sickle cell trait from both parents or sickle cell trait from one parent and another abnormal haemoglobin trait from the other parent. This is called recessive inheritance. A person who has sickle cell trait is unlikely to have any symptoms of sickle cell disease. However, they can still pass the trait to their children, and they are also at risk of having a child with sickle cell disease.
How common are sickle cell disease and sickle cell trait?
“Sickle cell disease affects approximately 100,000 Americans, but millions of people worldwide,” says Dr Creary. “Most of these individuals are from underrepresented minority populations1.” Although the disease can affect people of all racial and ethnic identities, it is particularly common among minority populations such as African Americans and Hispanics.
Sickle cell trait is much more common than sickle cell disease. Nearly 3 million African Americans have sickle cell trait. Despite the significant implications that it can have on future reproductive decisions, more than 80% of these individuals do not know or understand their sickle cell trait status.2
Why is it important for people to be tested for sickle cell trait?
“It is important for people to know their status so that they know if they are at risk of having children with sickle cell disease,” explains Dr Creary. Although people with sickle cell trait will not suffer from symptoms, they are at risk of having children with sickle cell disease and who can have severe health complications. If two people with sickle cell trait have a child, there is a one in four chance for each pregnancy to be affected by sickle cell disease.
Reference
https://doi.org/10.33424/FUTURUM457
© wavebreakmedia / Shutterstock.com
“It is also important to know that a parent with sickle cell trait and a parent with regular haemoglobin traits cannot have a child with sickle cell disease,” says Dr Creary. “It is important for parents to know whether they have sickle cell trait before they have children so that they can make an informed decision.”
What are the challenges of teaching parents about sickle cell trait?
As sickle cell trait is unlikely to cause any symptoms, many people carrying the trait may not know they have it or have even heard of it. The difference between sickle cell trait and sickle cell disease is also commonly confused, and many people struggle to understand that they are different.
“Parents of children with sickle cell trait often receive complex information about sickle cell trait and sickle cell disease at a time when they may be overwhelmed by caring for their newborn,” says Dr Creary. It is crucial that information is communicated in an accessible way so that parents understand the risks fully. To achieve this, Dr Creary and her colleagues have developed an education programme called SCTaware (sickle cell trait aware).
What is SCTaware?
SCTaware is an education programme that is delivered using videoconferencing. It was created to increase awareness about sickle cell trait among parents at high risk of having sickle cell trait. SCTaware was delivered as a videoconference so that people were able to access the information without having to travel to meet an educator.
The programme aimed to deliver information to parents in an accessible way and with visuals that were easy to understand. “We used tools to ensure that the language, pictures and format of our programme were presented clearly,” explains Dr Creary. “The programme also included an educator so that parents could ask questions, confirm that the information they received was clear, and confirm their understanding by teaching back the information that they learnt to the educator.”
What are the next steps for SCTaware?
Dr Creary and her team plan to conduct future studies to confirm that SCTaware improves sickle cell trait knowledge. “Our hope is that people are able to use this information to inform their future decision-making and share this information with their children with sickle cell trait, when they are old enough to understand it,” says Dr Creary.
1 US Centers for Disease Control and Prevention (www.cdc.gov/ncbddd/sicklecell/index.html)
2 Treadwell MJ, McClough L, Vichinsky E. Using qualitative and quantitative strategies to evaluate knowledge and perceptions about sickle cell disease and sickle cell trait. J Natl Med Assoc. 2006 May;98(5):704-10. PMID: 16749645; PMCID:PMC2569269.
 Dr Susan Creary
Dr Susan Creary
Hematology, Oncology and Blood and Marrow Transplant (BMT) Clinic, Nationwide Children’s Hospital, Columbus, USA
Field of research: Paediatric haematology
Research project: Raising awareness and knowledge of a poorly-understood genetic disorder within minority communities
Funder: US National Institutes of Health (NIH)
About paediatrics
Paediatrics is the branch of medicine that takes care of babies, children and young adults. This field is incredibly broad, reflecting the vast array of factors that contribute to a child’s health. For example, neonatal paediatrics focuses on the health of newborn babies, paediatric cardiology focuses on heart conditions that affect babies and young people, and paediatric endocrinology focuses on hormonal disorders such as those that might affect growth or puberty. Dr Creary’s research falls into the field of paediatric haematology, the study of blood disorders that affect babies, children and young people.
One field of paediatrics that Dr Creary is particularly excited about is preventive paediatrics. This looks at maintaining and promoting the health of children and young people to prevent complications, rather than waiting for and reacting to complications. Preventive paediatrics focuses on proactive steps that people can take to prevent their children from getting ill in the first place, such as routine check-ups, vaccines and education. “I hope that there are more opportunities for the next generation of paediatricians and researchers to increase effective use of preventative therapies and to implement these proven therapies into care,” says Dr Creary.
Pathway from school to paediatrics
• You should study science subjects at school and post-16-years-old, particularly biology and chemistry.
• It is also important to have a strong background in writing and ethics, so subjects such as English and philosophy may be useful.
• At college or university, take courses that develop your communication skills and understanding of how the circumstances in which people live, work, go to school, and socialise affect their health.
• In the US, the route to paediatrics will depend on the undergraduate degree you take. It is possible to study for a medical degree after gaining an undergraduate degree in a range of fields. For more information, see:
www.sgu.edu/blog/medical/how-to-become-a-pediatrician-a-step-by-step-guide
• In the UK, you will need to study a five-year undergraduate medical degree or a four-year postgraduate degree in medicine. For more information, see: https://www.healthcareers.nhs.uk/explore-roles/doctors/roles-doctors/paediatrics/paediatrician
Explore careers in paediatrics
• There are many different disciplines within the field of paediatrics, including community paediatrics, child mental health and paediatric emergency medicine. These disciplines are varied, and each requires specialised knowledge and training.
• Internships, work experience and volunteering are great ways to gain experience and boost your curriculum vitae (CV). Find out if your local university or hospital offers any such opportunities.
• To learn more about paediatric haematology specifically, the American Society of Hematology and The American Society of Paediatric Hematology/Oncology are useful organisations to learn from. They have training opportunities, summer experiences and mentoring programmes.
Meet Dr Creary
I have always enjoyed working with children. In medical school, I became interested in sickle cell disease because it affects every organ system, and I was looking for an opportunity to provide preventive care, rather than just treating complications once they happened. Paediatric sickle cell disease combined all these things into one career.
During my medical residency, I enjoyed my paediatric outpatient clinic because it served many children who were from underrepresented minority groups, and I also learnt that I enjoyed providing care to those with chronic diseases. Sickle cell disease aligned those interests and was scientifically fascinating to me. When I learnt more about the tremendous burdens this disease places on children, adolescents, young adults and their families, I realised that I had a great opportunity to make an impact.
I enjoy identifying the important questions that need to be asked and then designing the studies to try and answer them. It’s rewarding to know that the data we collect and the results we share may not only impact the children that I see in my clinic but also other children around the world who are living with this condition.
My proudest career achievements are when I completed my paediatric haematology/oncology fellowship, when I persevered through scientific rejection, and when I have had the opportunity to mentor young investigators in their work.
I hope to continue to expand the work that we are doing to increase knowledge about sickle cell trait and sickle cell disease so that individuals affected by these can make informed decisions about their health.
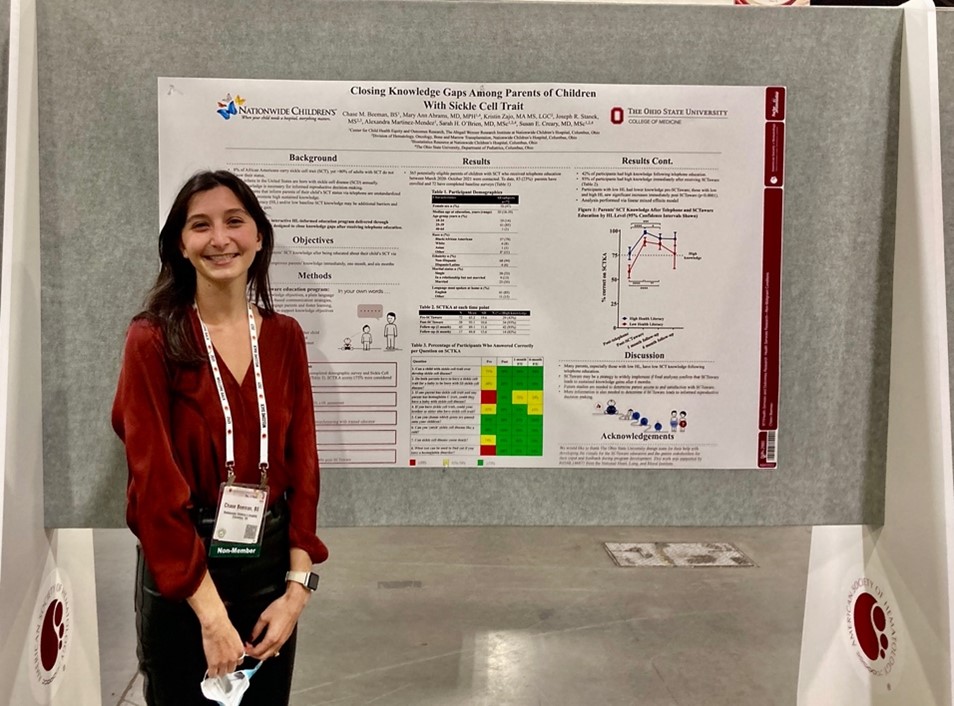
Meet Chase

Chase Beeman is a genetic counselling student at The Ohio State University. She focuses on family communication of and adaptation to genetic conditions.
I began working in research to gain experience in a medical field before returning to school for an advanced degree in healthcare. This was an exciting opportunity to help improve care and health outcomes for individuals with sickle cell trait and sickle cell disease. This work inspired me to pursue a career as a genetic counsellor.
I was the research coordinator and educator on SCTaware. I enrolled participants, provided the education, and tracked study progress. I also helped lead writing efforts for scientific manuscripts.
Learning how to be a sickle cell trait educator was a big challenge. This was a completely new skill for me, and it required me to learn a lot about sickle cell trait, sickle cell disease, genetic counselling, and health literacy. It taught me the importance of accessible and understandable patient education.
A highlight of the programme was seeing its impact on improving participants’ knowledge and confidence with complex health information. I look forward to seeing this programme evolve to reach a wider audience. I hope to see it inform future research on ways to improve sickle cell trait education.
As a soon-to-be practising genetic counsellor, I am excited to build a career in haematology genetics. I’d like to develop a clinical practice, counselling patients with inherited blood disorders.
Meet Dr Mary Ann Abrams

Dr Mary Ann Abrams is an assistant professor at The Ohio State University College of Medicine and primary care paediatrician at Nationwide Children’s Hospital.
I became a physician because medicine was so interesting and a wonderful way to help people. Throughout my medical training, I saw members of the health care team talking to patients using complicated words. Later, as a pediatrician, I led Reach Out and Read where we shared with parents the joy of reading aloud. All this led me to health literacy to help improve safety, quality, equity, and patient/family-centred care.
I helped plan, write, design and evaluate SCTaware to make sure we included plain language and ‘teach-back’ – explaining back using their own words. I trained people who delivered SCTaware, so using plain language and teach-back came naturally to them.
It has been great to see SCTaware being useful, acceptable and beneficial to parents. It helps make health care more equitable, safe and high quality. And it’s great that people I worked with are now health literacy champions!
I also use health literacy to work with teams to improve outcomes for babies born with cystic fibrosis or certain neuromuscular conditions. I partner with quality improvement to improve care for children with asthma on using their medicines; with dentists to make sure everyone knows when, how, where and why to come for dental care; and with psychiatrists caring for young people with depression. I also work with health equity and trained interpreters for patients with other languages or cultures, so all patients and families understand information we give them to care for their health.
My aim for the future is to make an impact in many settings, so that many people and organisations have health literacy skills.
Do you have a question for Dr Creary, Dr Abrams or Chase?
Write it in the comments box below and Dr Creary, Dr Abrams or Chase will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)

Learn about what happens when our blood production system fails:
www.futurumcareers.com/what-happens-when-our-blood-production-system-fails




0 Comments