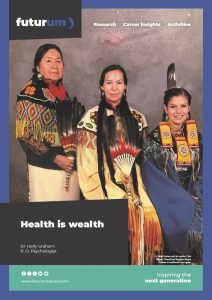
Health is wealth
Racism in healthcare is a serious barrier that prevents Indigenous peoples from receiving the care they need. At the University of Saskatchewan in Canada, Dr Holly Graham is supporting Indigenous nurses and nursing students, and she has developed a guide to empower healthcare professionals to address racism when they witness it.
Talk like a nurse
Cardiopulmonary resuscitation (CPR) — the lifesaving first aid technique of giving chest compressions and rescue breaths to circulate blood and oxygen when someone’s heart has stopped
Colonialism — the takeover and control of Indigenous lands and cultures by settlers
Culturally safe care — healthcare that is respectful, aware of the power imbalances and potential biases within the system, and ensures that patients feel safe and valued
Evidence-based care — medical decisions based on the best available scientific research, not personal opinions or stereotypes
Racism in healthcare can be a matter of life or death. In 2020, Joyce Echaquan, a 37-year-old Atikamekw woman, went to a Canadian hospital with stomach pain. Due to racial stereotyping, staff assumed she was a drug user despite there being no evidence for this. Joyce died two days later, while being abused by hospital staff. Racism and prejudice played a significant role in her death.
For Indigenous peoples in Canada (First Nations, Inuit and Métis), centuries of colonialism have led to earned deep mistrust in medical systems — and this mistrust still affects health outcomes today. When people do not feel safe or respected by healthcare providers, they are far less likely to seek medical help. As a result, health issues often go untreated until they become much more serious. And even when Indigenous patients do seek care, their concerns may be overlooked, their symptoms dismissed and their voices unheard.
“I have a second-degree black belt in karate,” says Dr Holly Graham, a Registered Nurse and member of the Thunderchild First Nation. “I was competitive and teaching in my own Dojo. Then in 2005, I started to have pain in my left knee, but my doctor just told me that I had arthritis and said there was no need to x-ray it.” After years of living with this pain and being dismissed by her doctor, Holly eventually managed to seek a second opinion in 2015, and she finally had an x-ray which revealed she had a rare condition that caused extra bones to grow in her knee joint.
“My example shows how First Nation peoples not only struggle to access emergency care due to the lack of trust in the healthcare system, but even when they see their doctor, their concerns are not taken as seriously,” says Holly. “If my doctor had x-rayed my knee when I first told him I had pain, I could have had surgery immediately instead of living in pain for years and losing the ability to run and practice karate.” Holly’s story is not unique. It highlights how racism in healthcare is not always about life-or-death emergencies — it is also about being ignored or mistreated in ways that quietly damage people’s health over time.
Saving lives with CPR
The tragic death of Joyce Echaquan deeply affected Holly. “I asked myself, ‘As a nurse, what can I do to make sure this never happens again?’” Around the same time, Holly had been watching the TV show Grey’s Anatomy. “Everyone who comes into hospital in Grey’s Anatomy seems to be given CPR (cardiopulmonary resuscitation),” says Holly. “CPR can save lives, and I wanted to create a plan to save lives lost related to racism. So, I decided I’d use the same acronym – CPR – to highlight the urgency of addressing racism in healthcare.”
Holly created the CPR RACISM guide to help healthcare professionals address racism:
- Call out, how can I help?
- Plan and practice your intervention strategy
- Review the chart, speak to and assess the client
- Review the client’s treatment plan and politely ask for the reason(s) for the current approach
- Advocate for and educate yourself about anti-racism and practice allyship
- Check with the client and listen to their concerns, be the safe person
- Intervene, always be an active bystander
- Speak up about your concerns and get support for yourself
- Model safe, competent and compassionate care

The guide draws on interventions Holly has been using since the beginning of her nursing career in the 1980s, when she worked in the US and witnessed racism directed at Black patients and colleagues. Her mentor, Dr Verna St. Denis, helped shape her thinking about race and education. As Holly progressed through her nursing career, she realised many of her colleagues did not know how to intervene when they witnessed racism or how to teach nursing students to combat racism.
The CPR RACISM guide offers a clear approach: “If a nurse thinks a client is not receiving appropriate care, they should review the client’s chart themselves and listen to the client, then consider what evidence-based care they need based on their symptoms,” says Holly. “When speaking out against racist behaviour, it’s important to target the behaviour not the person – labelling someone as a racist in the moment is never helpful.”
Promoting the Seven Sacred Teachings
The Seven Sacred Teachings (Spiritual Laws) are guiding values that help people live in balance with themselves, others and the world around them. These teachings – love, respect, courage/bravery, honesty, wisdom, humility and truth – are rooted in Indigenous knowledge systems and can be applied in everyday life to build better relationships. “Loving yourself allows you to love others,” says Holly. “Respect is about honouring all living things. Courage helps us speak up when something is wrong and do the right thing, even when it’s hard. Honesty is speaking from the heart, holding and keeping your promises. Truth is your key to freedom. Humility is related to being humble and reminds us to get up after we tumble. And wisdom comes from listening and the lessons we learn through our experiences. When people live according to these values, we will have healthier relationships and can build healthier communities.”
These Indigenous values are at the heart of CPR RACISM. “To me, the Seven Sacred Teachings are embedded in the CPR RACISM guide because it is about promoting these values for all of creation and humanity,” says Holly. Just as the teachings encourage us to act with honesty, courage and humility in our relationships, the guide calls on healthcare professionals to reflect on their actions, listen to patients and intervene when they witness injustice.
Supporting Indigenous nurses
Indigenous nurses often face unique challenges during their education, training and careers – and many of these come from a clash of worldviews. “The Western model traditionally views health very much on the physical level, but the Indigenous view of health encompasses physical, mental, emotional and spiritual wellness,” explains Holly. “If, as a nurse or nursing student, you are told that how you see the world is wrong or doesn’t apply to medicine, then it is hard to stay in a profession that doesn’t respect your beliefs.”
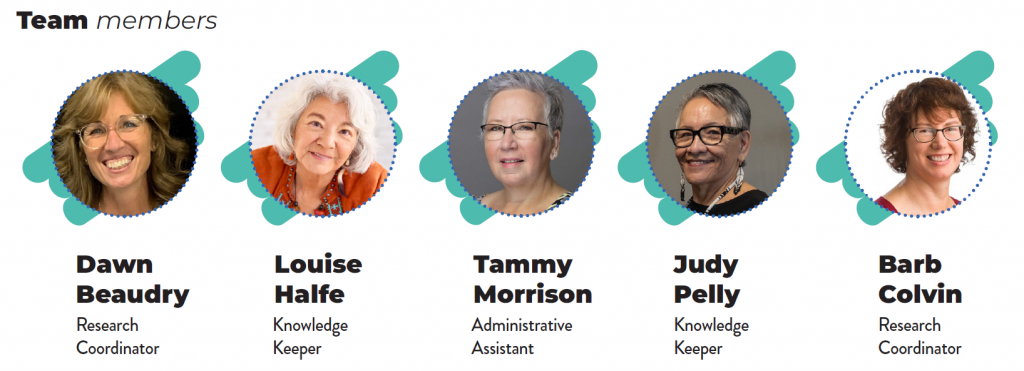
To help address this, Holly created the kā-wīci-pimohtēmāt Professional Nursing Practice Group – a network where Indigenous nurses can connect, share their experiences and feel supported. The group also works directly with the provincial regulatory body to shape healthcare policies related to Indigenous peoples in Saskatchewan. Anti-racism education and training is now a required part of Canadian nursing education. “This means that nursing graduates will be better prepared to provide culturally safe care and have the skills to address racism in healthcare settings,” says Holly.
Holly is also the project manager for the miyo mashihkêwiyiniwak (Good Medicine People) space at the University of Saskatchewan. “This new research space was created to address health disparities for Indigenous peoples and to centre Indigenous worldviews,” she says. “The Seven Sacred Animals that represent the Teachings are etched on a glass wall as you enter this space.”
Through her work addressing racism and supporting Indigenous nurses, Holly is building a brighter future for healthcare in Canada. “Patients feel more comfortable if they can identify with their healthcare professionals,” she explains. “Indigenous nurses are uniquely positioned to understand the needs of Indigenous patients because we have shared understandings of history, culture and belief systems. We need more Indigenous nurses if we want to address health disparities and ensure everyone can feel safe in healthcare.”
 Dr Holly Graham
Dr Holly Graham
R.D. Psychologist
Professor in Psychiatry, College of Medicine, University of Saskatchewan, Canada
Registered Nurse and Registered Doctoral Psychologist
Fields of research: Nursing education, Indigenous health
Research projects: Addressing mentorship and reconciliation with a focus on creating safety for Indigenous peoples to access healthcare
Funders: Canadian Institutes of Health Research (CIHR); Saskatchewan Health Research Foundation (SHRF); Canadian Nurses Foundation (CNF); Canadian Foundation of Innovation (CFI); Department of Psychiatry, College of Medicine, University of Saskatchewan
Pathway from school to nursing
At high school, study biology, chemistry and mathematics to build essential knowledge about the human body and medical science, and to develop problem-solving skills that are vital in nursing practice.
At university, a degree in nursing will prepare you for a clinical career as a Registered Nurse.
“Engage with nurses and other healthcare professionals and try to shadow them in their work,” advises Holly. “Attend career days and volunteer in healthcare settings like long-term care facilities.”
Take opportunities to work with people, such as helping with youth groups or community-based activities. “Nursing is all about developing relationships with people,” says Holly. “You will have to deal with people who are unwell and unhappy, so you need to enjoy working with others.”
Explore careers in nursing
Nursing is a very flexible career. You can work with people of all ages, from babies to elderly patients, and in a huge range of places, from hospitals to mental health clinics to community health centres. And you can specialise in whichever area most interests you, such as emergency care, oncology (cancer) or mental health.
“It is a huge privilege to care for others when they are in need and to share in a small part of their journey through life,” says Holly.
“Health is wealth,” says Holly. “When you don’t have health, it’s hard to appreciate the rest of life. And one of the benefits of being a nurse is that you learn how to improve your own health.”
These videos share personal stories of Indigenous nurses who graduated from the University of Saskatchewan, inviting you to consider a career in nursing: youtube.com/playlist?list=PLUaewQzUIZwpw1afWztcnq3X44tAa8YDU
Meet Holly

Reference
https://doi.org/10.33424/FUTURUM619
When I graduated from high school, I wanted to be a police officer then go into law. But I was only 17, so I wasn’t old enough to start police training. My mother was a Certified Nursing Assistant, and it was her dream that one of her children would become a Registered Nurse. She suggested I take a two-year nursing programme so I could stay in school until I was old enough to get into Police College.
I never wanted to be a nurse because I was terrified of needles – I used to faint whenever I had injections! But I decided to enter the nursing programme to keep my mom happy and I thought I’d just drop out when we started to give needles. But when it came to it, I discovered that I didn’t mind giving needles to other people. So, I stayed in the programme and, when I graduated, I realised that nursing was a good fit for me because I enjoyed caring for people. I’ve now been a nurse for 40 years!
I enjoy the fact that nursing is both a science and an art. There’s the science of anatomy, physiology and pharmacology. But there is also an art to how you deliver care, communicate with your patients and make them feel safe.
My family has felt the impact of colonialism and racism. My mother was sent to a residential school, but she never spoke about it, so I didn’t know anything about her experiences. She refused to teach us the Cree language because she said we would have a better chance to succeed in life if English was our first language. As a child, I never understood why Indigenous peoples were poorer than the white people around us – I thought that Santa must like white children better because he gave them better gifts.
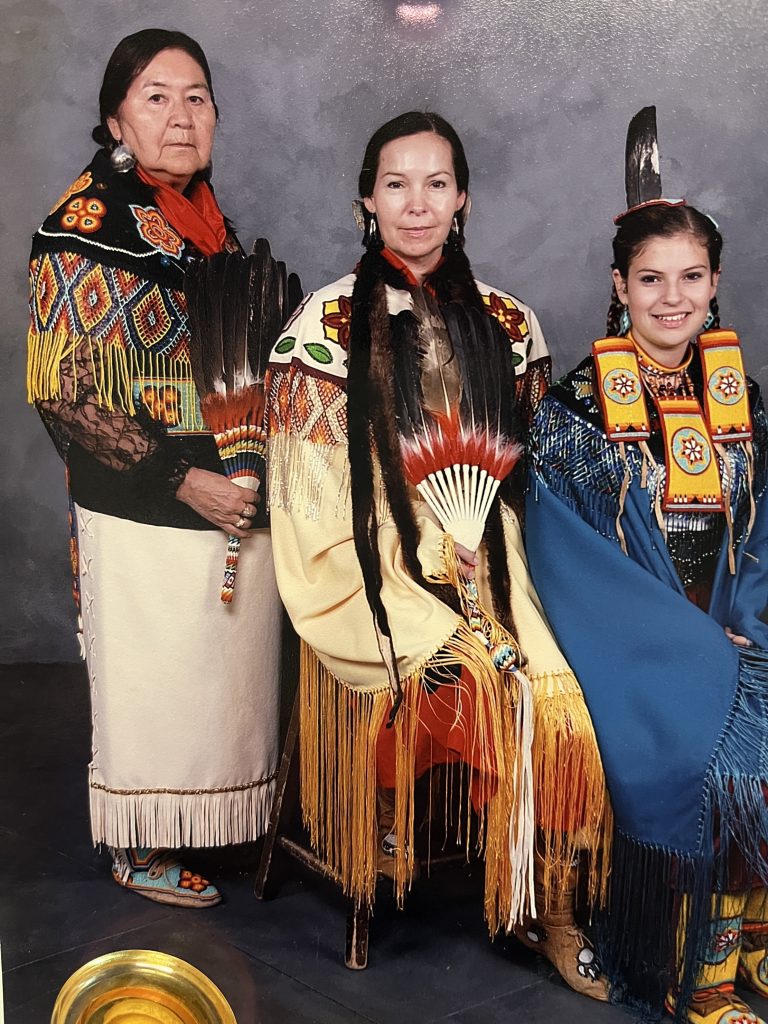
From an early age I participated in Cree cultural traditions, such as Sundances, Pow Wows and Sweats. Participating in Sundances has been central to the development of my spirituality. I was given my Cree name, okimāwahtik-iskwēw, at a Sundance when I was eight by a blind Elder who had dreamt of me. He said it was an important name with a lot of responsibility, and that I would bring peace and happiness to those around me.
Do you have a question for Holly?
Write it in the comments box below and they will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)
Discover how the Ktunaxa Nation is ensuring that health services honour Ktunaxa culture, language and worldviews:


















0 Comments