What causes problems with the lower urinary tract?
Our bodies are fascinatingly interconnected. Did you know that urinating a lot at night might be due to a heart problem? Or that a condition such as diabetes might affect urination? In the US, a team of doctors and researchers, including Professor Cindy L. Amundsen from Duke University School of Medicine, have come together to study lower urinary tract dysfunction, which affects almost 70% of people over 60 years old. The scientists’ aim is to understand what causes lower urinary tract symptoms and how treatment outcomes for these conditions can be improved.
TALK LIKE A UROGYNAECOLOGIST
Bladder — the organ that stores urine
Gynaecology — the area of medicine focused on treating female diseases, especially those that affect the reproductive organs
Obstetrics — the area of medicine focused on pregnancy, childbirth and female health immediately after delivery
Pelvic — related to the pelvis, the space between the hips where several organs and structures are located
Urethra — the tube through which urine leaves the body
Urinary tract — the organs that make urine and remove it from the body, including the kidneys, ureters, bladder and urethra
Urogynaecology — a specialised field of gynaecology and urology that focuses on female pelvic medicine
Urology — the area of medicine focused on diseases of the male and female urinary tract
Our urinary tract involves all the organs that work together to make urine and remove it from our bodies. This includes the kidneys, where urine is made; the ureters, which carries urine to the bladder; the bladder, where urine is stored; and the urethra, through which urine exits the body. The urinary tract is divided into two parts. The upper urinary tract includes the kidneys and ureters, and the lower urinary tract includes the bladder and urethra.
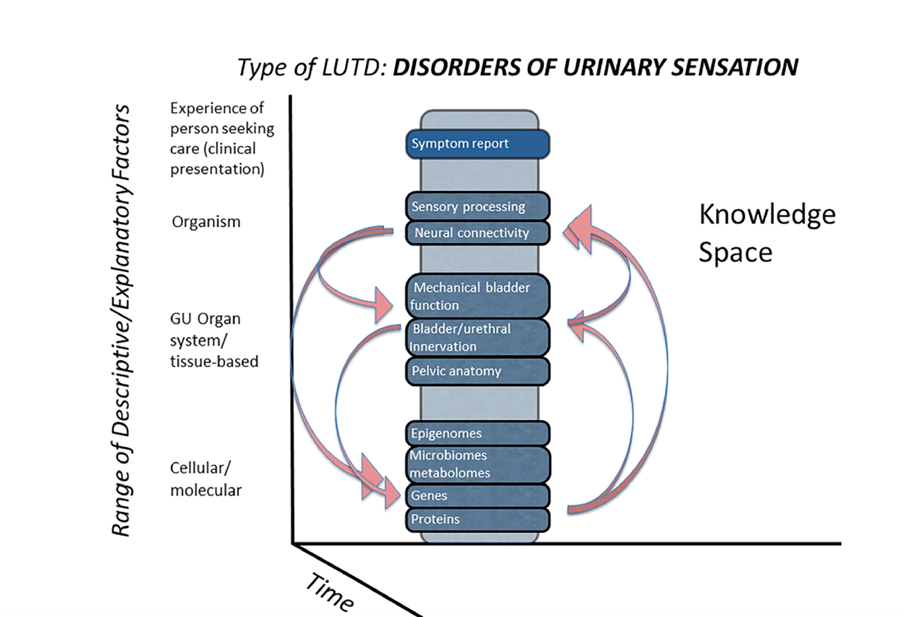
When the lower urinary tract is not working properly, someone might have lower urinary tract dysfunction (LUTD). Both males and females can experience LUTD, as can children of any age. LUTD encompasses a broad range of different problems, and symptoms can include leaking urine, having sudden urges to pee, urinating at night, having a slow stream or feeling as if your bladder is not empty after urinating.
As you can imagine, the symptoms of LUTD can greatly impact an individual’s day-to-day life. At Duke University School of Medicine, Professor Cindy L. Amundsen is studying LUTD with the goal of developing better treatment options for people struggling with this condition. “Symptoms can limit activities people enjoy doing outside the home, reduce their social interactions, disrupt sleep, and decrease their feeling of mental and physical wellness,” says Cindy.
Can lower urinary tract dysfunction be treated?
Luckily, there are many therapies that already exist which can treat the symptoms of LUTD. Sometimes, patients can improve their symptoms by decreasing the amount of caffeine they drink, reducing the amount of fluid they drink, or limiting drinking fluid before going to bed. Other patients might do exercises to strengthen the muscles around the urethra and bladder or undergo surgery to support the urethra. “Additional treatments involve placing an electrode near nerves that control the bladder or injecting medicine into the bladder to decrease the muscle spasms,” explains Cindy.
However, there are limitations to these treatments. The first limitation is that urinary symptoms are often attributed to the lower urinary tract when the symptoms may not be related to problems with the lower urinary tract at all. Symptoms of LUTD can occur due to poor sleep, the amount of fluid being consumed, childbearing, previous surgeries, ageing or certain medications. “They can also be caused by non-urological organs and diseases or conditions such as diabetes, anxiety or depression,” explains Cindy. It can be difficult to diagnose exactly why someone is experiencing symptoms, which can reduce the effectiveness of the treatment.
“Another limiting factor is that many patients experience a combination of symptoms, so treatment that focuses on a single symptom may result in suboptimal care,” explains Cindy.
To improve these treatment outcomes, Cindy has received grant funding from the US National Institute of Health (NIH) to support research to help understand the different subtypes of lower urinary tract symptoms and the causes for each group.
How is Cindy studying LUTD?
Cindy is part of a team of surgeons, biological scientists, computational scientists and medical research professionals who have come together from six different universities across the US to study the lower urinary tract and improve treatments for LUTD. The network was formed in 2012 and named ‘LURN: the Symptoms of Lower Urinary Tract Dysfunction Research Network’. It is supported by grants from the US National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Institutes of Health’s National Center for Advancing Translational Sciences 5U01-DK097780-09.
Crucially, the project involves people from various backgrounds who are all experts in different areas. Since lower urinary tract symptoms (LUTS) can have multiple causes, the research project needs to have a diverse team whose members can share their knowledge on various areas.
The scientists within LURN work with patients struggling with urinary symptoms. “We gather information through questionnaires, physical examinations, and urine and blood samples,” says Cindy.
The goal is to be able to group patients with similar symptoms together into subtypes and analyse the differences between these groups. To do this, the team created a new questionnaire called LURN SI-29 and a shortened version, LURN SI-10. “While there are several questionnaires available to clinicians, none capture the full spectrum of LUTS in both men and women which could then be used as a tool for both clinical use and research,” explains Cindy.
How does a country-wide research programme like LURN work?
The two main challenges of having a collaboration across the US are logistics and expense. The whole group of scientists meets virtually twice a month and in person in Washington, DC, four times a year to discuss their findings. The varying time zones across the country mean that organising virtual meeting times can be difficult and enabling the whole team to travel is expensive.
So, why has LURN decided that a country-wide research project is worth it? The main reason is that it allows the team to recruit a large and diverse group of patients. “This makes the findings of our study more generalisable to others across the country and even to those in other countries who have similar symptoms,” explains Cindy.
What has the project found?
The initial research that has come out of LURN shows that not only are there different symptoms among patients, but also differences in demographics, medical conditions and biological variables between patients.
Cindy and the rest of LURN used advanced statistics to group individuals together into subtypes according to the similarity of their symptoms. Interestingly, they found that symptom improvement varied by subtype, meaning that some subtypes responded better to therapies than others.
What is next for LURN?
The LURN team aims to understand which specific treatments work best for each subtype. In order to do this, the researchers need to recruit more patients with LUTS and perform more studies to understand the underlying causes of symptoms. “By incorporating more data that include diagnostic information and possibly cellular or molecular factors, more meaningful differences among patients may be identified,” says Cindy.
The LURN team also plans to use computer modelling techniques to estimate the risk of individuals developing LUTS later in life, with the goal of preventing more cases. The team hopes its results can be used to develop better, personalised treatment plans, so that more people struggling with lower urinary tract symptoms will be able to get the help they need.
 Professor Cindy L. Amundsen, MD
Professor Cindy L. Amundsen, MD
Roy T. Parker Endowed Professor of Obstetrics and Gynecology, Division of Urogynecology, and Professor, Department of Surgery, Division of Urology,
Duke University School of Medicine, USA
Fields of research : Obstetrics and Gynaecology, Urogynaecology
Research project: Improving treatment outcomes for lower urinary tract dysfunction
Funders: US National Institute of Diabetes and Digestive and Kidney Diseases, US National Institutes of Health’s National Center for Advancing Translational Sciences
Funder of Futurum Careers project: Roy T. Parker Endowed Professorship, Duke University School of Medicine
Reference
https://doi.org/10.33424/FUTURUM396
Unless stated otherwise, all images © Cindy L. Amundsen
About urogynaecology
If you enjoy learning about women’s issues and think you will enjoy a medical career, then working in gynaecology could be for you. Gynaecology is often combined with obstetrics to create the field of obstetrics and gynaecology, referred to by the acronym OB/GYN. Having a strong knowledge of both areas will make you more able to solve problems related to women’s health.
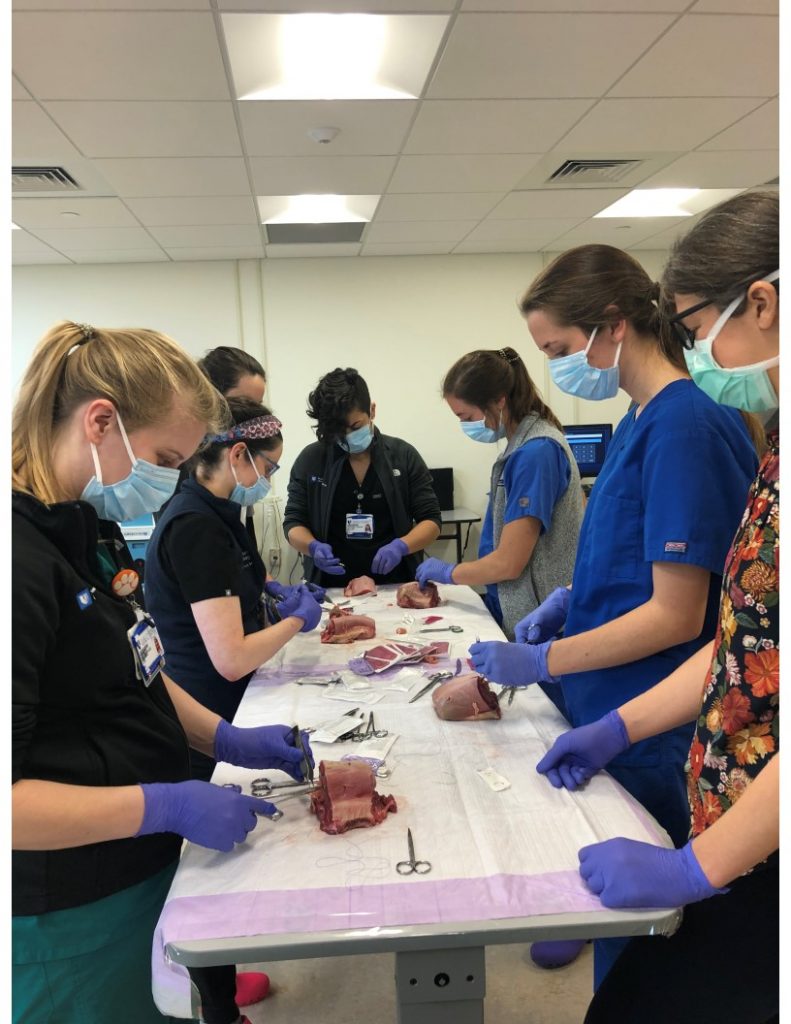
Gynaecologists are medical doctors who perform surgery and who have undergone specialised training to become experts in the female reproductive system. They might work in a clinical environment, engaging daily with patients experiencing health problems and/or work in a research setting, conducting experiments or surveys to better understand medical problems and develop new, innovative treatments.
You must be curious about women’s health issues to work in this field, as there is still so much to be discovered. “We still don’t understand why women get many of the gynaecologic conditions such as endometriosis, recurrent urinary tract infections, chronic pelvic pain, fibroids, infertility, gynaecologic cancer, menstrual irregularities, pelvic support problems, urinary incontinence, and many more conditions,” explains Cindy.
Future gynaecologists will pursue research questions to understand what contributes to the onsets of these conditions and diseases, as well as how they progress and what treatments might be possible. Gynaecologists also need to be able to disseminate their findings to the wider scientific community and use their results to improve advice for patients.
Cindy wears multiple professional ‘hats’. As a researcher, surgeon, clinician and educator, she highlights the different aspects to careers in this field: investigating issues and aiming to find clinical solutions, working directly with patients, and helping to train and support the next generation of gynaecologists.
How are new technologies aiding Cindy’s work as a surgeon?
“Robotic surgery allows for very complicated surgery to be done with more precision, flexibility and control than open surgery as it is performed through very small incisions,” says Cindy. “Additionally, technologic advances with medical devices allow surgically implanted devices to be placed with less anaesthesia and through smaller incisions. Finally, the accuracy of radiographic and other diagnostic technologies has improved so much that we are detecting earlier stages of medical conditions which allows for minimally invasive treatments to be performed.”
Pathway from school to gynaecology
• During high school and post-16-years, study biology, chemistry, physics and mathematics. Working in OB/GYN also involves having strong interpersonal and communication skills, so taking language courses can be very useful too.
• To work in gynaecology, you must complete a medical degree before undergoing specialised training in obstetrics and gynaecology. If you are attending university in the US, you will need to do a pre-med degree before you start studying medicine.
• If you have the option to choose courses during your university degree, Cindy recommends studying deductive reasoning, psychology, communication, epidemiology, ethics, anatomy, biochemistry, pathophysiology, pharmacology, pathology and immunology. “In addition, math skills that will help would be algebra, geometry, statistics and probability,” she adds.
• Cindy recommends the website Career Girls, which has a fantastic page on working in obstetrics and gynaecology, details of what an average day might involve, and interviews with various obstetrics and gynaecology role models.
Explore careers in gynaecology
• “Working in gynaecology is very rewarding, but it is a demanding career and, thus, you must be passionate about the field,” says Cindy. “Gynaecologists will see patients in the clinic and operate at the hospital, so every day will be different. Skills that would be useful are dexterity, patience, communication, problem solving, flexibility, resilience, organisational skills and physical stamina.”
• If you are interested in working with women’s health issues but do not want to be a gynaecologist, then there are lots of other options too. Nurses, midwives, general practitioners and psychologists, as well as jobs within non-profit organisations and women’s centres, all play important roles in improving women’s health.
• Indeed.com has some useful information on working in obstetrics and gynaecology, including which skills you need to develop to be successful in this career.
• According to the US Bureau of Labour Statistics, the average annual salary for obstetrics and gynaecology in the US is $277,000
• Cindy recommends watching this 15-minute video by Med School Insiders about what it is like to work in OB/GYN: So You Want to Be an OB/GYN [Ep. 22]. There is also an accompanying blog post.
Meet Cindy
I was first inspired to pursue a career in gynaecology because I grew up sewing my own clothes with my mother and sister; I always enjoyed working with my hands. Sewing, in many respects, is like performing a surgery. You must understand the anatomy or material you are working with, know the techniques necessary to perform the task, and have the creativity and skill to finish the procedure/ product. In medical school, I was drawn to the specialty of surgery and wanted to improve women’s health conditions that require surgery. I did additional training to become a urogynaecologist, one who specifically performs reconstructive pelvic surgery involving the lower urinary tract organs and gynaecologic organs.
Three major experiences of my childhood led me to be a researcher, surgeon and educator. As expressed above, my mother taught me to sew at a very young age – cutting out the patterns and sewing with my hands. My father taught me to be a good researcher as I would watch him read dental manuals and journals. Lastly, when I was a teenager, I learned how to become a dance instructor. Teaching others gave me much satisfaction, so I wanted a profession where I could also teach what I know.
Balancing research, surgery and education during my work is not easy, and it can get very busy. There are times I need to prioritise tasks, so staying organised and preparing ahead of time to meet specific deadlines is very important. I am passionate about all three areas and strive to do my best in each of them.
They all interconnect. When I am performing surgery, I have several trainees in the operating room and educate them on the surgical techniques and other clinical aspects. My research often involves clinical trials that involve the recruitment of patients, so I get them involved and educate my patients on the advances and improvements in patient care discovered through research.
I find it very gratifying to pass on knowledge, skills and wisdom to the next generation, and I enjoy helping my mentees achieve more than they could do alone. Mentees also challenge me, helping me stay abreast of newest developments!
The worst piece of advice I was ever given was that I was told there was no need for me to work hard when I first came on faculty, since I had a very successful and world-renowned surgeon as a husband. This did not fit my personality and so I disregarded it, worked hard, and became successful in my own right.
Outside of work, I enjoy training for sprint triathlons and playing golf. To relax, I love doing puzzles and playing mah-jong and bridge.
I feel very grateful that over the past 24 years, my involvement in research, patient care and trainee education has enabled me to make contributions that have significantly impacted the quality of patient care. In 2017, I was awarded the Rodney Appell Continence Care Champion, one of the most prestigious recognitions in the field of continence care. In addition, in 2021, I received the Duke School of Medicine Career Mentoring Award in Clinical Research/Population Health which recognised excellence in research mentoring.
Cindy’s top tips
1. Be curious and open to the opportunities that are presented to you, no matter how small they may seem.
2. Follow the 4 Ps:
– When given an opportunity – PERFORM. Do the best that you can.
– Nothing that is worth something is easy, so be PATIENT and learn from any mistakes that you make.
– PERSEVERENCE is very important to achieve your goals.
– Lastly, follow your PASSION, even if someone says you should pursue something else.
KURe – the K12 Urologic Research Career Development Program
As part of her commitment to education and mentoring other scientists, Cindy leads Duke University School of Medicine’s KURe Program * which supports researchers to build independent research careers. We meet three programme participants.
* funded by the NIH/National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK) K12-DK100024-11
Meet Cassandra

Dr Cassandra Kisby, MD
Duke Division of Urogynecology, Assistant Professor of Obstetrics and Gynecology, Duke University School of Medicine
Fields of research: Obstetrics and Gynaecology, Urogynaecology
Funders: K12 Urologic Research Career Development Program K12-DK100024-11 NIH/NIDDK
The most impactful thing that has changed my career path has been mentor relationships. There are people who will tell you it can’t be done; find the people that believe in you and will help you navigate the unbeaten path. I am from a very small town in North Carolina and am the first in my family to go to college. A very special high school physics teacher believed in me and sponsored me for a full tuition scholarship to Duke and it changed my life.
Because I am a clinician-scientist, my research covers both basic science and clinical research. I am a urogynaecologist, meaning I treat women with bladder and pelvic issues, so my research is aimed at improving care for women with these issues. For my current research, I am using regenerative medicine technologies (such as stem cells) to help women who have pelvic floor disorders or were born with differences in bladder and gynaecologic anatomy. As a clinician-scientist, I have a diverse research profile – I even do some work that involves 3D printing. The key is to find a meaningful question or problem and think creatively.
Success requires persistence. A hypothesis is an educated guess and, statistically, hypotheses cannot all be correct. If you are following your passions and doing work that is meaningful to you, you will be more resilient when you are faced with negative results (when your hypothesis was wrong).
Like many things in life, the most challenging part of research is finding funding. The great idea is just the start – you have to write well-written grants to be able to fund the research projects. The writing and planning is worth it when you have a research breakthrough. It’s great to synthesise your results and present them to your peers at national meetings and publish your results in an academic journal.
The KURe Program has given me time and funding to develop my research career. I have time to prepare and conduct my research studies and meet with a career coach, and the ability to network with other young researchers at Duke. It has been a remarkable programme, and I am very thankful to have such support from mentors like Dr Amundsen.
As part of my clinical training, I did fellowship in urogynaecology. During fellowship, I decided I had a special interest in urogenital congenital anomalies, meaning anatomic differences of the bladder and genitals in women. For example, some women can be born with a double uterus. Over the last two years at Duke, I’ve created a Congenital Anomaly Program, which has grown into a multi-disciplinary treatment programme. It was featured in the Duke OB/GYN magazine.
My hope is to share my research and clinical skills with the next generation of clinician-scientists; the future is very bright.
Cassandra’s top tips
1. Learn about the differences between mentors, sponsors and career coaches. At each stage of your career, I would find a few with whom you can form formal relationships.
2. Sometimes the cost of education can be a barrier. Seek out local and national scholarships to prevent debt from driving your career decisions.
3. Look into summer programmes at local colleges and universities. These are a great way to network and get exposed to science and research.
Meet Eric

Dr Eric Gonzalez, PhD
Department of Biomedical Engineering, Duke University, USA
Field of research: Neuroscience
Funders: K12 Urologic Research Career Development Program, and K01 Research Scientist Development Award K12-DK100024-11 NIH/NIDDK
The Duke KURe Program and Dr Amundsen helped kick start my translational research programme. Making my research objectives relevant to human conditions made me stand out compared to having only pre-clinical studies.
My research is currently focused on developing a peripheral nerve stimulation device to manage LUTS and improve bladder emptying in underactive bladder (UAB). I hope to increase our understanding of the muscular and neural alterations in the lower urinary tract that may accompany UAB and provide a foundation for clinicians to develop innovative therapeutics to improve patient outcomes.
We began a clinical pilot study, mentored by Dr Amundsen, to determine the influence of bladder and urethral electrical stimulation on bothersome symptoms and bladder function in adult women with UAB. This is the first step in developing alternative therapeutics.
It is challenging navigating your career and differentiating your research enough to receive funding. It is rewarding working on solutions to problems that many older adults face.
The Duke KURe Program provided an opportunity to collaborate with clinicians and develop mentorship in clinical research. It also provided protected time to support collecting preliminary data for my next awarded grant.
I am proud of being awarded an NIH Mentored Research Scientist Development Award to support four years of my research. For the future, I plan to continue pursuing a career in clinical research.
You can get your foot in the door by volunteering to help in a laboratory.
Meet Byron

Dr Byron Hayes, PhD
Department of Pathology, Duke University School of Medicine, USA
Field of research: Pathology
Funder: K12 Urologic Research Career Development Program K12-DK100024-11 NIH/NIDDK
Around halfway through my time in graduate school, my research shifted focus to my current studies involving the nervous system, which was a new field of interest for the lab in which I currently work. This has been particularly enjoyable since I like having the opportunity to drive a new research interest forward.
Currently, my research focuses on discovering better treatment options for patients that suffer from frequent urinary tract infections (UTIs) by using mice. I am specifically interested in treating pain and other symptoms that relate to the nervous system.
My key successes include developing a mouse model of UTI induced pain and urinary frequency, which enabled me to discover what goes on in the bladder after a UTI. The next step is to use this mouse model to study anxiety and depression, since these are other symptoms experienced by patients.
A lot of my time is spent designing experiments and going through trial-and-error as these are unanswered research questions. Fortunately, when discoveries are made, it gives you a strong sense of accomplishment, knowing that you have contributed to your field of research.
The KURe Program has enabled me to interact with several clinicians; these interactions are very important in ensuring that my research is directed at areas that are relevant to UTI patients.
I was vital in expanding my lab into neuroscience during graduate school. My work also awarded us research funds (~$1.5 million) to further support our studies. These are two achievements I am very proud of.
I plan to start my own research lab in the future, studying interactions between the nervous system and bladder after infection. I will focus on the bladder and brain/ spinal cord, since the bladder is regulated by the brain.
Byron’s top tip
Start working in a lab early. This is important so you can truly learn whether it’s the right path for you. If it is, you will be able to start getting the right guidance to make your path forward clearer.
Do you have a question for Cindy, Cassandra, Eric or Byron?
Write it in the comments box below and Cindy, Cassandra, Eric or Byron will get back to you. (Remember, researchers are very busy people, so you may have to wait a few days.)










Cindy: Can you supply any research papers that deal with minumum LUTD and treatment with Estradiol for elderly women?
Thanks for any references.
Hi Nancy,
Here are a few articles. One is a review articles discussing vaginal estrogen use, another a cochrane review comparing vaginal estrogen and systemic estrogen as they relate to treating LUT symptoms, and the other a randomized trial comparing a medication for OAB vs. vaginal estradiol. I hope this helps. There are papers on the benefits for preventing recurrent urinary tract infections with the use of vaginal estrogen and how the urogenital microbiome changes/improves with vaginal estrogen use. Relationships are being made between a “healthy” microbiome and bladder function and it is thought that estrogen plays a role.
Shifren.Jan. Genitourinary Syndrome of menopause. Clinical Obstetrics and Gynecology. September 2018. 61 (3): p 508-516.
Cody June, Jacobs Madeleine Louisa, Richardson Karen, et al. Oestrogen therapy for urinary incontinence in post-menopausal women. Cochrane Database Syst Rev. 2012 Oct 17;10(10).CD001405.
doi: 10.1002/14651858.CD001405.pub3.
Ellington DR, Szychowski JM, Malek JM, Gerten KA, Burgio KL, Richter HE. Combined Tolterodine and Vaginal Estradiol Cream for Overactive Bladder Symptoms After Randomized Single-Therapy Treatment. Female Pelvic Med Reconstr Surg. 2016 Jul-Aug;22(4):254-60.
Hi Cindy and team, I am a patient suffering from underactive bladder. Did a whole lot of MRI and CT Scans for the past 8 months since diagnosed through urodynamics procedure in May 2023. The causes are not neurogenic or myogenic. It is classified as idiopathic. No medical procedure nor medication which can reverse the issue except that I was given Tamsulosin by the urologist to help manage the symptoms daily. It does affect the basic quality of life both mentally and emotionally. Very unfortunately, UAB is not very well researched or spoken about in the medical world after I read up so much about the chronic condition. I was wondering if there are any new advances or proven medication in treating or improving this condition. If only there was a breakthrough innovation in this area, it will probaby relieve and save hundreds of millions of patients suffering in silence when diagnosed early. Thanks !
Hello Eugene,
I am sorry to hear about your UAB condition. Although no obvious myogenic or neurogenic cause can be attributed to the etiology of your UAB, loss of the ability of the bladder to contract well is the focus of ongoing research. As you can see in my article, research with biomedical engineers who can develop various forms of stimulators may result in the ability to stimulate directly the nerves in the urethra and/or bladder resulting in improved function of the underactive bladder. I agree current medications such as the one you are on only try and relax the urethral muscles so that an underactive bladder muscle might be able to empty better. As you mention, the medications are suboptimal and likely neurostimulation will be the answer in the future.
Thank you very much Dr Cindy ! I hope there will be a breakthrough in the next few years with clinically proven results which will change and bring back the basic quality of life for my of the patients like me having to live with this condition with unknown causes. I am also wondering if these are some post covid or vaccine effects which created the issues.